Description #
This unit will describe the correct administration, scoring and interpretation of the Visual Analogue Scale (VAS) for Pain performed for TJA patients.
Learning Objectives #
By the end of this unit, the learner will be able to perform the following tasks for TJA patients:
– Administer the Visual Analogue Scale (VAS) for Pain
– Score the Visual Analogue Scale (VAS) for Pain
– Interpret the Visual Analogue Scale (VAS) for Pain
What is this test? #
What is the Visual Analogue Scale for Pain? #
The Visual Analogue Scale (VAS) for pain is a valid, reliable, and responsive measure with no reported ceiling or floor effects that is useful for assessing THA and TKA patients. The VAS falls within the WHO’s ICF domain of Body Function/Structure (Figure 1) because it assesses a single dimension measure of joint-specific or global pain intensity at rest or with activity. In addition, it can be administered relatively quickly requiring a total of approximately 1 minute to complete and score.
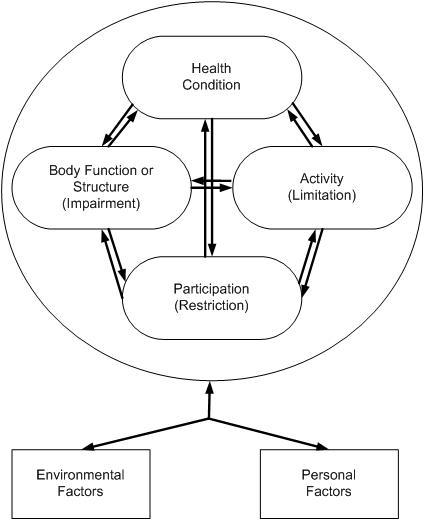
Figure 1. The International Classification of Functioning, Disability and Health (ICF) Conceptual Model. Taken from Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. Figure 2-1.
When do I use it? #
When do I use the Visual Analogue Scale for Pain? #
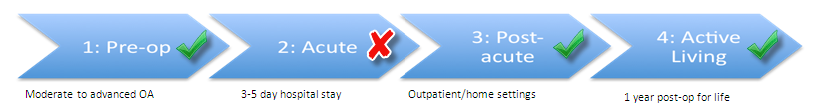
The Visual Analogue Scale (VAS) for pain can be used in all the phases along the TJA Continuum of Care. Indeed, as you can see in Figure 2, it is recommended for use in the Pre-Operative, Acute, Post-Acute, and Active Living phases of the TJA continuum. Health professionals can therefore use this outcome measure to monitor change in the patient’s status as he or she moves across all phases of care.
Figure 2. The phases along the TJA Continuum of Care for which the VAS is recommended.
Equipment needed? #
What equipment is used to complete the Visual Analogue Scale for Pain? #
For the patient to complete the Visual Analogue Scale (VAS) for pain, the following equipment is required:
- A paper copy of the VAS
- Pen
- Ruler with millimetre increments
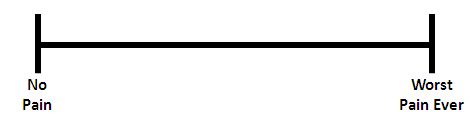
Figure 3. The Visual Analogue Scale.
CLINICAL TIPS!
- Whenever you are using the VAS, you may wish to note what pain medications the patient is taking as pain medication can affect the patient’s VAS score!
How do I do it? #
How do I administer the Visual Analogue Scale for Pain? #
It is simple to administer the Visual Analogue Scale (VAS) for pain. Instruct the patient to place a single mark on the line between the two end points to indicate how much pain they are currently feeling. The far left left line or anchor, indicates “No pain” and the far right anchor indicates “Worst pain ever.”
IMPORTANT LINKS!
- Do you want all the module information on a single piece of paper? If so, click this link! → VAS One Pager
How do I score it? #
How do I score the Visual Analogue Scale for Pain? #
Scoring the Visual Analogue Scale (VAS) for pain is easy to do4:
- Using a ruler, measure the distance in mm from the left hand “no pain” anchor to the mark that the patient makes on the line.
- Record the value between 0-100 mm
REMEMBER!
- Visual Analogue Scale (VAS) for pain is not suitable for persons with visual or cognitive impairment, or for telephone administration.
What does it mean? #
How do I interpret the Visual Analogue Scale for Pain? #
It is simple to interpret the Visual Analogue Scale (VAS) for pain – the higher the score, the more intense the pain. For example, the recommended cut points for patients with post-surgical pain are:
- No pain: 0-4 mm
- Mild pain: 5-44 mm
- Moderate pain: 45-74 mm
- Severe pain: 75-100 mm5
Furthermore, did you know that CLINICALLY MEANINGFUL CHANGE can be indicated by a reduction of as little as 13 mm or more of a patient’s VAS score? It’s true! It has been established that the:
MCID is 13 mm if the initial VAS score was 34 mm or less7,8
- What does this mean for my patient? It means that the change in score between test occasions must be greater than or equal to 13 mm (when the initial score was less than or equal to 34 mm) in order to indicate that a clinically meaningful change has occurred.
MCID is 28 mm if the initial VAS score was 67 mm or more7
- What does this mean for my patient? It means that the change in score between test occasions must be greater than or equal to 28 mm (when the initial score was greater than or equal to 67 mm) in order to indicate that a clinically meaningful change has occurred.
- To avoid error in interpretation, ensure that the VAS line measures 100 mm after printing or photocopying.
Examples #
Example 1 #
Mr S is post- op day 1 after a THA. On initial assessment, you measure Mr. S’s pain to be 94 mm on the VAS. After 2 days of PT treatment, Mr. S is being discharged home and his pain is 54 mm on the VAS.
Has there has been a clinically meaningful change in Mr. S’s pain?
*The MCID is 28 mm when the initial VAS score is 67 mm or greater.
1. Calculate the change between test occasions
94 mm – 54 mm = 40 mm
2. Compare the MCID to the change in score between test occasions
40 mm > 28 mm
Yes, clinically meaningful change has occurred as the change in test scores between test occasions is greater than the MCID of 28 mm.
Example 2 #
Mr S is now 14 days post op after his THA and is attending your clinic. On initial assessment, Mr. S’s pain is 33 mm on the VAS. After 1 week of treatment, Mr. S reports that his pain is 21 mm on the VAS.
Has there been a clinically meaningful change in Mr. S’s pain?
*The MCID is 13 mm when the initial VAS is 34 mm or less.
1. Calculate the change between test occasions
33 mm – 21 mm = 12 mm
2. Compare the MCID to the change in score between test occasions
12 mm < 13 mm
No, clinically meaningful change has not occurred as the change in test scores between test occasions is less than the MCID of 13 mm.
References #
- Gagliese L, Weizblit N, et al. The measurement of postoperative pain: a comparison of intensity scales in younger and older surgical patients. Pain. 2005;117(3):412-20.
- Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976;2(2):175-84.
- McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: a critical review. Psychol Med. 1988;18(4):1007-19.
- Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27(1):117-26.
- Hawker GA, Mian S, et al. Measures of adult pain. Arthritis Care Res. 2011;63(Suppl 11):S240-52.
- Finch E BD, Stratford PW, Mayo NE. Physical Rehabilitation Outcome Measures. 2 ed: Canadian Physiotherapy Association; 2002.
- Bird SB, Dickson EW. Clinically significant changes in pain along the visual analog scale. Ann Emerg Med. 2001;38(6):639-43.
- Todd KH, Funk KG, et al. Clinical significance of reported changes in pain severity. Ann Emerg Med. 1996;27(4):485-9.
- WHO International Classification of Functioning, Disability, and Health – http://www.who.int/classifications/icf/icf_more/en/
- Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. F.A. Davis Company: Philadelphia.
