Thoracocentesis is a surgical procedure performed for the removal of fluid such as exudate, blood or air from the pleural cavity.
Topographical Anatomy
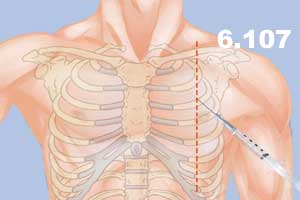
In the intercostal space (between 2nd and 3rd rib) the needle insertion or incision should be made at the upper margin of the rib in order to avoid damage to the neurovascular intercostal bundle (vein, artery, nerve) located in subcostal groove.
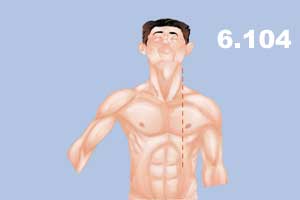
Anteroposterior projection
- 2nd intercostal space anteriorly at the mid-clavicular line to remove air (Figure 6.104 -6.105).
- skin
- subcutaneous tissue and fascia (in females, it also includes mammary glands)
- superficial pectoral fascia
- external intercostal fascia
- external intercostal muscle
- internal intercostal muscle
- innermost intercostal muscle
- parietal (costal) pleura
- pleural cavity

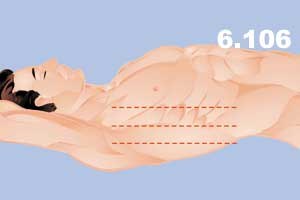
For the removal of fluid, the location is posterior or mid-axillary line on 5th or 6th intercostal space (Figure 6.106).
- skin
- subcutaneous tissue
- latissimus dorsi (for posterior axillary line) and serratus anterior (for mid-axillary line)
- external intercostal fascia
- external intercostal muscle
- internal intercostal muscle
- innermost intercostal muscle
- parietal pleura
- pleural cavity
Needle Aspiration Techniques #
a) The patient must be in a comfortable sitting position with hands comfortably lying on a table in front of them.
b) Posterioanterior and lateral x-rays as well as careful percussion are needed to localize the level of fluid or air.
c) Prep and drape using aseptic techniques.
d) Infiltrate with xylocaine (1:10,000 epinephrine).
e) Insert the needle (Figure 6.107 – 6.108).

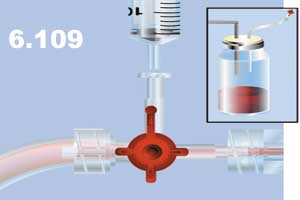
f) Attach a three-way stopcock to the needle and connect it to the collecting reservoir (Figure 6.109). Withdraw with the fluid in the syringe and empty it to the reservoir.