Description #
This unit is designed to help health care professionals develop a better understanding of respiratory suctioning skills.
Learning Objectives #
Upon completion of this module you will be able to:
- Explain the mucociliary clearance and the impact of retained secretions in the lung.
- List the indications for tracheal suctioning
- Discuss the complications associated with tracheal suctioning
- Demonstrate the correct technique for tracheal suctioning through a stoma or tracheostomy tube
- Demonstrate the correct technique of tracheal suctioning through a pharyngeal airway
Introduction #
SUCTIONING IN RESPIRATORY CARE
This unit is designed to help you develop a better understanding of respiratory suctioning skills, and explores airway suctioning in a variety of different contexts. Airway suctioning is an important skill in respiratory care. It is necessary to maintain a patent airway, remove saliva, pulmonary secretions, blood, vomitus, or foreign material and is undertaken in acute hospital and community settings.
Mucociliary Clearance and the Impact of Retained Secretions in the Lung #
Mucociliary cells line most of the respiratory tract from the nose to the terminal bronchioles. This layer of pseudo-stratified cells contain thousands of fine hair-like structures called cilia. Cilia move rhythmically at a rate of 1200 beats/minute to help propel mucous and contaminants from the lungs up toward the mouth for clearance. The cilia found in the nasopharynx beat downwards towards the mouth.
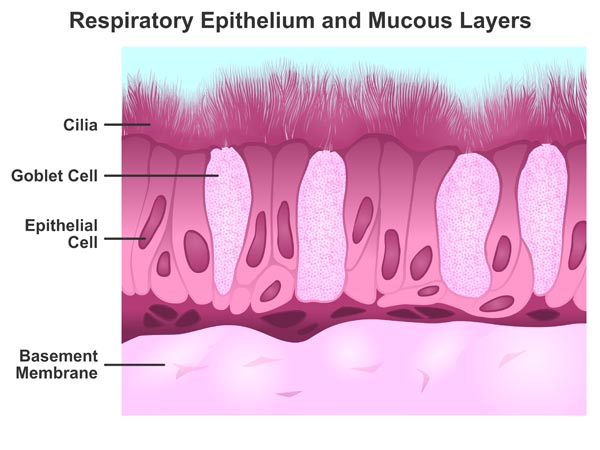
Mucous is produced by goblet cells and submucosal glands in the lung. It covers the ciliated epithelium as a thin, discontinuous blanket. The blanket consists of two layers: the top, thick viscous layer called the ‘gel’ and the bottom, thin fluid layer called the ‘sol’. Inhaled particulate matter and contaminants deposit on the gel layer of the mucuous. The cilia move freely in the sol layer to help propel the thicker gel layer along up to a rate of 10 mm/min in the large airways. Normally, between 10 and 100 ml of mucous per day is moved by this mucociliary transport mechanism up to the mouth and is coughed out or swallowed.
The efficiency of mucous clearance can be impacted by excess or very thick mucous production, or by interfering with ciliary activity.
Retention of secretions can result in the following complications:
1. Increased airway resistance
- Expiration is generally passive, relying on the normal elastic recoil of the thorax. Mucous accumulation in the large airways can slow down expiratory flowrates, resulting in air trapping in the lungs and hyperinflation. Hyperinflated lungs increases the risk of pneumothorax and interferes with normal pulmonary gas exchange.
- Increased Work of Breathing
- Increased resistance in the airways means a patient increase their effort to inhale and exhale. Hypoxemia and worsening gas exchange will cause a patient to increase their respiratory rate to compensate.
2. Hypoxemia/Hypercapnia
- Mucous that accumulates in the alveoli will impede oxygen and carbon dioxide transfer across the alveolar capillary membrane, resulting in decreased oxygen levels and retention of carbon dioxide in the blood.
3. Atelectasis
- Retention of secretions can result in blockage of the small airways of the lung. This can cause collapse of alveoli and sometimes an entire lobe distal to the blockage.
4. Infection
- Mucous that is not cleared from a lung can trap contaminants and result in purulent infections. Infections can in turn contribute to hypoxemia.
The Indications for Tracheal Suctioning #
There are three key indications for tracheal suctioning:
1. To maintain a patent airway and remove saliva, pulmonary secretions, blood, vomitus, or foreign material from the trachea as evidenced by:
- Visible secretions in airway
- Coarse inspiratory/expiratory crackles or gurgling heard on auscultation
- Feeling of secretions in the chest during palpation
- Suspected aspiration of gastric or upper airway secretions
- Increasing respiratory distress or agitation
- Decreasing oxygenation status
- Radiographic evidence of retained secretions resulting in atelectasis or consolidation
2. To stimulate cough
- To check reflexes in patients with decreased level of consciousness
- In patients unable to cough due to changes in mental status or the influence of medication
3. To obtain a sputum sample for lab analysis
- To identify and treat pulmonary infection or disease
The Complications Associated with Tracheal Suctioning #
1. Hypoxemia
- Hypoxemia is the most common complication associated with suctioning. When a negative pressure is applied to the lungs, air and oxygen are removed along with secretions. Hypoxemia is generally preventable with preoxygenation with 100% oxygen prior to suctioning. A continuous pulse oximeter is recommended during tracheal suctioning, and pausing to reoxygenate between suction attempts will help to ensure vital sign stability. Limiting the length of time negative pressure is applied will also help to prevent hypoxemia.
2. Cardiac Arrhythmias
- Tachycardia as a result of suctioning generally occurs secondary to hypoxemia or patient agitation. Mechanical stimulation of the larynx or trachea with a suction catheter could result in vagal stimulation, leading to bradycardia or hypotension. Hypotension may also occur with severe coughing episodes that decrease venous return. If signs of arrhythmias or hypotension occur, the suction catheter should be immediately withdrawn and oxygen and ventilation given as needed.
3. Atelectasis
- Tracheal suctioning can remove air from the lungs along with secretions, causing alveolar collapse or atelectasis. This can be minimized by limiting the amount and duration of negative pressure during the suction procedure. The outer diameter of the suction catheter has a significant effect on atelectasis – a catheter that is properly sized to be a smaller diameter than the airway will entrain some air from the room during suctioning. A catheter that is too large will block the airway and entrain air from the lungs, causing atelectasis. It is recommended that the external diameter of the catheter should never exceed one half to two thirds of the diameter of the airway.
4. Mucosal Trauma
- Trauma to the airway mucosa can occur due to the rigidity of the suction catheter as it passes along the soft tissues of the airway. Lubrication of the catheter with sterile water-soluble lubricant or saline and preventing use of excessive force when advancing the catheter will help to prevent trauma. Damage may also be caused by catheters adhering to the tracheal wall during suctioning. Limiting the negative pressures to –100 mmHg to –120 mmHg will make the catheter less likely to pull tissue away from the mucosa when the catheter is withdrawn.
5. Infection
- Contamination of the lungs is likely when a catheter is passed through the upper airway and into the lungs during nasotracheal suctioning. This procedure should be avoided if possible on immunocompromised patients. The risk of infection during tracheal suctioning can be minimized by using proper sterile technique. Suction catheters are disposable and should not be reused.
6. Increased Intracranial Pressure
- Increased intracranial pressure can occur in susceptible patients, secondary to coughing or hypertension.
7. Laryngospasm
- Tracheal suctioning through a nasal or oropharyngeal airway can cause laryngospasm when the suction catheter passes through the larynx. If the patient exhibits signs of laryngospasm (stridor, fits of uncontrolled coughing, decreased SpO2) the catheter should be immediately withdrawn and the patient given oxygen. A physician and respiratory therapist should be contacted before suction attempts are resumed.
8. Aspiration
- Tracheal suctioning through a nasal or oropharyngeal airway can trigger a strong gag reflex if the catheter accidentally passes into the esophagus. If vomiting occurs, turn the patient to their side and suction the mouth immediately. Monitor vital signs and contact a physician and respiratory therapist before suction attempts are resumed.
The Technique for Suctioning Through a Stoma or Tracheostomy Tube* #
The Technique for Tracheal Suctioning Through a Pharyngeal Airway* #

Suctioning Simulation* #
The screen below is an interactive simulation that explores the management of airway suctioning therapy in the acute clinical setting.

PATIENT PROFILE:
Name: Mrs. Alexandra Kostasan,
Alexandra Kostasan 42-year-old female with advanced-stage Amyotrophic Lateral Sclerosis(ALS), a rapidly progressive, invariably fatal neuro-logical disease that attacks the nerve cells (neurons) responsible for controlling voluntary muscles. The patient was diagnosed with ALS 3 years ago at the age of 39 and is now considered to be in the end stage of the disease.
History Leading to Current Complications:
The patient has had a fever for two days and an increase in sputum production. She has had difficulty swallowing her saliva lately and now feels like she cannot clear her phlegm effectively. The patient lives at home and has a care aid to help with daily care. She had a PEG tube for feeding inserted three months ago due to dysphagia. She has been diagnosed with pneumonia.
Current Orders:
- 1.5mg Scopolamine patch Q3 days to reduce saliva
- Avelox antibiotic 400mg OD
- Oxygen to keep SpO2 92% Effexor
- 75mg OD Ativan
- 1mg sublingual Q4H PRN
- Daily chest physiotherapy
- Daily physiotherapy for range of motion
References #
- Egan’s Fundamentals of Respiratory Care – Fifth Edition, Scanlan CL, Spearman CB, Sheldon RL. C.V. Mosby Company 1990
- Respiratory Care Equipment – Branson RD, Hess DR, Chatburn RL. J.B. Lippincott Company 1995.
- Respiratory Therapy Equipment – McPherson SP, Spearman CB. C.V. Mosby Company 1990.
- Vancouver Acute Patient Care Guideline N-020 Nasopharyngeal Airway: Insertion, Care of and Removal. 1998.
- Vancouver Acute Patient Care Guideline S-300 Suctioning: Oronasopharyngeal. 1999.
- Vancouver Acute Patient Care Guideline T-195 Tracheostomy: Suctioning 2003.
- Vancouver Acute Respiratory Services Policy RT-SER-16 Suctioning and Specimen Collection. 2000.
