Description #
This unit will describe the correct administration, scoring and interpretation of the Stair Climb Test (SCT) performed for TJA patients.
Learning Objectives #
By the end of this unit, the learner will be able to perform the following tasks for TJA patients:
– Administer the Stair Climb Test (SCT)
– Score the Stair Climb Test (SCT)
– Interpret the Stair Climb Test (SCT)
What is this test? #
What is the Stair Climb Test? #
The Stair Climb Test (SCT) is a valid1, reliable3,4, and responsive5 measure of functional strength, balance, and agility1 that is useful for assessing THA and TKA patients. In addition, the SCT also falls within the WHO’s ICF domain of Activity (Figure 1) and can be completed relatively quickly requiring approximately 2 minutes to administer and score1,2,6.
 #
#
Figure 1. The International Classification of Functioning, Disability and Health (ICF) Conceptual Model. Taken from Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. Figure 2-17.
When do I use the Stair Climb Test? #
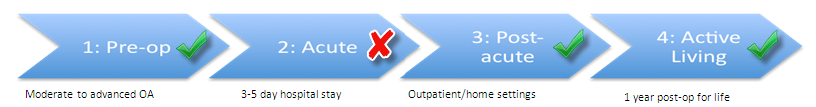
The Stair Climb Test (SCT) can be used in a number of phases along the continuum of care. Specifically, as seen in Figure 2, the SCT is recommended for use in the Pre-Operative, Post-Acute, and Active Living phases of the TJA continuum. Health professionals can therefore use this outcome measure to monitor change in the patient’s status as he or she moves through these phases of the care (*note that it is not recommended in the Acute phase).
Figure 2. The phases of the TJA continuum of care for which the SCT is recommended.
Equipment needed #
What equipment is used to perform the Stair Climb Test? #
To perform the SCT with a patient, the following pieces of equipment are required2:
- Stairs with 8-14 steps (step height of 16-20 cm) and handrails
- Stopwatch
- The patient’s usual walking aid if they use one
REMEMBER!
- When possible, it is recommended the test be performed on a 9-step stair case with a handrail and 20cm (8 inch) step height2.
How do I administer the Stair Climb Test? #
- A written version of the instructions can be found at the following link → Instructions
How do I score it? #
How do I score the Stair Climb Test? #
Scoring the SCT is easy to do:
- Measure the total time it takes the patient to ascend and descend the steps.
- Record the time to the nearest 100th of a second.
Use of any walking aid and handrail (for ascending/descending or both) is permitted and recorded2.
What does it mean? #
How do I interpret the Stair Climb Test? #
It is simple to interpret the SCT: the faster a patient can safely ascend and descend the stairs the better. Furthermore, did you know that a TRUE CHANGE is indicated by an improvement of only 5.5 seconds in patients with advanced hip and knee OA awaiting TJA (9 steps) and 2.6 seconds in patients after TKA (11 steps)3,4? It’s true! It has been established that the:
MDC is 5.5 sec in patients with advanced hip and knee OA awaiting TJA (9 steps)4
- What does this mean for my patient? It means that the change in score between test occasions must be greater than 5.5 sec in order to reflect a true change and not just measurement error.
MDC is 2.6 sec in patients after TKA (11 steps)3
- What does this mean for my patient? It means that the change in score between test occasions must be greater than 2.6 sec in order to reflect a true change and not just measurement error.
Example 1 #
Mr S has come into your clinic to improve his strength and balance prior to his upcoming TKA. On initial assessment, Mr S’s Stair Climb Test (SCT) score was 17.6 seconds on a 9 step stair case (no gait aid or railing was used). After 6 weeks of treatment, Mr S’s SCT score was 11.1 seconds. Determine if there has there been a true change in Mr. S’s SCT score?
1. To determine if there has been a true change, calculate the change in score between test occasions
17.6 sec – 11.1 sec = 6.5 sec
2. Compare the MDC to the change in score between test occasions. *MDC = 5.5 sec
6.5 sec > 5.5 sec
Yes, true change has occurred because the difference between test occasions is greater than the MDC of 5.5 sec.
Example 2 #
Mr. S is now 3 weeks post op for TKA and is being visited by community PT. On assessment, Mr S’s SCT score was 21.4 seconds on a 11 step stair case with 2 railings (Mr. S used one railing to both ascend and descend the stair case). After 1 week of treatment, Mr S’s SCT score was 19.6 sec (Mr. S used one railing to both ascend and descend the stair case). Determine if there has been a true change in Mr. S’s SCT Score?
1. To determine if there has been a true change, calculate the change in score between test occasions
21.4 sec – 19.6 sec = 1.8 sec
2. Compare the MDC to the change in score between test occasions. *MDC = 2.6 sec
1.8 sec < 2.6 sec
No, true change has not occurred because the difference between test occasions is less than the MDC of 2.6 sec.
References #
- Bennell K, Dobson F et al. Measures of physical performance assessments. Arthritis Care Res 2011;63(S11):S350-S370.
- Dobson F, Hinman RS et al. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthritis Cartilage 2013;21:1042-52. Manual available at: www.oarsi.org/sites/default/files/docs/2013/manual.pdf
- Almeida GJ, Schroeder CA, et al. Interrater reliability and validity of the stair ascend/descend test in subjects with total knee arthroplasty. Arch Phys Med Rehabil. 2010;91(6):932-8.
- Dobson F, Hinnman RS et al. Measurement properties of performance-based measures to assess physical function in hip and knee osteoarthritis: a systematic review. Osteoarthritis Cartilage 2012;20:1548-62.
- Kennedy DM, Stratford PW, et al. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord. 2005;6:3.
- WHO International Classification of Functioning, Disability, and Health – http://www.who.int/classifications/icf/icf_more/en/
- Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. F.A. Davis Company: Philadelphia.
