Description #
An introduction to patient-centered care will be presented as a holistic method of caring for patients about to undergo a surgical procedure. The topics of professionalism, communication/ collaboration, teamwork and leadership will be discussed in relation to perioperative nursing care. Overview of the roles of the Perioperative LPN and registered nurse, both the scrub role and the circulating role, will be discussed in detail.
Learning Objectives #
At the end of the session the LPN will be able to:
- 1. Define Perioperative nursing as set down by the ORNAC standards
- 2. Describe how using patient-centered care – the nursing process, standard nursing care plans and clinical pathways can be tailored to meet the individual needs of the patient in the operating room
- 3. Recognize & utilize professionalism in perioperative nursing practice
- 4. Recognize & utilize methods of effective communication practices in the perioperative nursing setting
- 5. Recognize & utilize methods of effective teamwork in the perioperative nursing setting
- 6. Describe the role of the scrub nurse and the circulating nurse and how each fit into the scope of practice of the licensed practical nurse
Much has been written, across many disciplines of healthcare, about patient centered care (PCC). It is seen as a worldwide standard of care and is part of the core philosophy underpinning the VCH Perioperative Nursing Program. Patients undergoing specific surgical procedures will require certain nursing care, for example, all patients will require positioning during surgery and all the related nursing interventions surrounding positioning to keep the patient injury free. In order to provide PCC, the perioperative nurse must look beyond the label of a patient’s condition or the surgery they are scheduled to receive and see the patient as a whole person.
The perioperative nurse must use their knowledge and skills to apply the nursing process to each individual patient, enabling them to develop a plan of care that is unique to that patient.
- To look at the patient
- To assess that patient
- To realize that the person in front of you is not just a case that requires instruments or a particular piece of equipment
The patient is a person who is frightened about surviving surgery and what the outcome of that surgery might be The patient is a person who is worried about how they will cope later, or how friends will treat them if they lose their independence, and so on. You are the support person who is with them at possibly the most frightening time of their entire surgical hospital stay. It is your responsibility to assess them, to modify your plan of care to suit their needs, to communicate their needs and problems to the other members of the operative team and above all to give them your undivided attention and support while they are awake and while they are asleep – under an anesthetic – and to relay the information to those looking after the patient postoperatively to ensure continuity of care.
Just remember the few minutes you spend with each and every patient, and their family member, will make a difference for them and rest assured, they will be comforted by the words… “I am your nurse and I’ll take good care of you.”
Exercise One
Read the case study history below. You are the perioperative nurse responsible for the care of Agnes Smith while she is undergoing an operative procedure (abdominal hysterectomy): a) Identify the specific knowledge you will need in order to provide her with patient-centered care. b) Identify the specific nursing skills/ techniques you will need in order to provide her with patient-centered care.
Exercise Two
Identify the problems/issues (actual and potential) specific to Agnes Smith that are of concern to the perioperative nurse. Briefly list the problems you have identified in the form of nursing diagnoses (actual and/or potential). Hint: Using patient centered care Agnes can be seen holistically. If you are having trouble formulating a nursing diagnosis in the correct format, watch the following video – How to Write a Nursing Diagnosis (Note: NANDA refers to the North American Nursing Diagnosis Association – a compilation of approved nursing diagnostic terminology).
Exercise Three
Expanding on the nursing process – as described in Alexander’s: nursing diagnosis, planning (desired patient outcome), nursing intervention/ implementation, evaluation (actual or desired) – choose one of the nursing diagnoses related to Agnes, from exercise two, which may cause an alteration to your standard plan of care for an abdominal hysterectomy patient.
Case Study – Agnes Smith
Agnes Smith is a 78 year old petite lady who has a huge uterine fibroid. The fibroid has been causing her trouble and is the reason that has made her seek medical care and has resulted in an impending surgical intervention. She has osteoporosis that isn’t too bad yet – she’s found it in time and is now taking drugs and extra calcium. Agnes has always been able to
cope with anything that has come up. She has been the center point of her family. She has accomplished many goals in life that she has set out to do and she is content with getting older so long as she has her health. She is a widow, and has been for the last 6 years. She has a married son in Toronto and a son and daughter-in-law that live in town – she does not get along with the daughter-in-law very well. She has 3 grandchildren and they are the loves of her life, and luckily she sees them often. When her husband died rather suddenly from a heart attack, her daughter-in-law bought her a dog to keep her company. The dog gets her out on walks every day, rain or shine…. Daisy has become a constant companion. Agnes spoils her badly and loves her and since her husband’s death she has also become involved with a book club at the seniors centre. She has the occasional lunch there and goes regularly to play bridge. She also takes an exercise class at the gym twice a week as she thinks it probably helps her osteoporosis. Agnes isn’t really a religious person, but believes in the general principle that one should be kind and respectful and tread lightly
on the rest of the universe. She is convinced that there is some higher presence that governs things, so she goes to the Anglican church where she was brought up. She reads a lot about other religions and cultures and lately has taken up meditating. She is busy balancing everything, the bridge playing, the book club, the exercise program, the invitations out for coffee which have resulted from the going to the senior’s center, the visits from her grandchildren and the responsibility of her dog. Agnes might say she is more involved and busier now than she was when her husband was alive…although some evenings are long and lonely.
Agnes’ beliefs are the law she lives by. She is a kind lady, it’s reflected in everything she does for her family and her friends and in return kindness is given back to her. Agnes has been able to continue a relatively normal life with her osteoporosis, her exercise helps and so do the drugs and the extra calcium. But the uterus thing…well that’s been the thing that’s brought her down. Post menopausal bleeding combined with numbness in her right leg, caused by pressure from the fibroid, has just been too wearing on her and it has started cutting into her activity level. It is obvious to her and her dog Daisy that walks have become less frequent.
Her daughter-in-law has been after her to go to the doctor. Even her friends have noticed a difference in her energy level. Her son has made the appointment for her and is accompanying her to the office visit, where Agnes learns the only way to alleviate her problem is an abdominal hysterectomy under general anesthesia. Agnes is worried about being confused after the anesthetic, and about not being able to cope with the pain. Will she be able to have a bowel movement after the surgery or will it be too painful? Will she be able to void or will she need a catheter for a prolonged time? Will the staff in the OR handle her carefully enough to prevent breaking her brittle bones?
Will she be able to get comfortable in bed postoperatively…and what if it’s cancer!!! Who will look after her dog while she is incapacitated? She has already made up her mind…”I won’t have surgery if I can’t find someone to look after Daisy”. “How will I get my groceries in, my daughter-in-law and son live so far away and they work and don’t really have time for this”. To top it all off, her friend came over the other day and told her what a terrible experience she had in hospital the last time she was in. Agnes’ heart may stop during anesthesia, the fibroid may turn to cancer, she may hemorrhage postoperatively or she may do just fine and regain the full spectrum of her life.
What’s next? #
We will be using patient-centered care throughout the program – it will be touched on in PN 003 -preoperative assessment; and every time you encounter a patient in the full-time clinical program. You will plan for each surgical procedure to ensure positive outcomes for the patient and tailor your nursing interventions to achieve these outcomes based on your patient-centered care nursing diagnoses of each individual patient you have the privilege to care for.
Learning Objectives #
At the end of the unit the student will be able to:
- Define professionalism
- Have an understanding of the history of perioperative nursing
- Describe the characteristics of a profession
- Describe the elements that make perioperative nursing a distinctive specialty within the nursing profession
Recommended readings:
- Canadian Council for Practical Nurse Regulators (CCPNR) – Standards of Practice & Competencies for Perioperative Licensed Practical Nurses – Part One & Part Two.
2. College of Licensed Practical Nurses Scope of Practice
- Review the content in the navigational links in the right hand column.
- Learn more about the professional associations that govern and/or guide professional practice in the operating room. Become familiar with the following websites (and their publications/ journals), as they will be useful in answering future practice questions and providing education:
- Operating Room Nurses Association of Canada (ORNAC) and its provincial equivalent the Perioperative Registered Nurses Association of BC (PRNABC)
- College of Licensed Practical Nurses of BC (CLPNBC)
- Licensed Practical Nurses Association of British Columbia (LPNABC)
- Canadian Council for Practical Nurse Regulators (CCPNR)
- Canadian Nurses Association (CNA)
- Association of Perioperative Registered Nurses (AORN)
History of Perioperative Nursing #
In the 1800’s the succession of war expanded the scope and experiences of nurses, as demonstrated by the work of Florence Nightingale in field hospitals and the conception of surgical conscience and aseptic technique.
The specialty of perioperative nursing emerged in the 1880’s as the number of surgeries increased and surgeons recognized the need for nurse assistance. Schools helped to change the concepts of the time, that nursing was a subservient and menial profession. Many physicians believed the Nightingale model ‘over-trained’ nurses to be ‘above’ themselves! – posing a threat to a well established physician authority.
Two world wars projected nurses’ work into the national limelight as their contribution of service in the armed forces and volunteer organizations, such as the Red Cross, achieved public interest and recognition. In the mid 1940’s post war nurses returned home and wanted to retain many of their expanded responsibilities: anesthesia assistance, prepping of the surgical patient, control of asepsis, care of the OR environment and supplies, supervision of OR personnel and assisting the surgeon in surgical procedures.
Eventually, OR nurses began to organize their members, pool professional knowledge and share ideas and in 1949 in New York City an independent association of OR nurses was formed which later became, the Association Of Perioperative Registered Nurses (AORN). In Canada similar organization of OR members began, first in Quebec, in 1958 and later in BC, in 1966, with the British Columbia OR Nurses Group (BCORNG). BCORNG disaffiliated from CRNBC in 2009 (due to legislation from the Health Professions Act) to form the Perioperative Registered Nurses Association of BC (PRNABC). From this followed the formation of the Operating Room Nurses Association of Canada (ORNAC) in 1983 with membership from 6 provinces, including BC. Today there is also a Canadian Council for Practical Nurse Regulators (CCPNR) which have recently been proposed a set of standards and competencies for Perioperative LPNs (2010). Since the 1960’s, our profession has gained purpose, goals and new trends. Our focus continues to support nursing education, recruitment and retention, development of standards of practice and an OR credentialing model.
What is a Profession? #
Definition of Professionalism #
The main factors that deferentiate a profession from an occupation are:
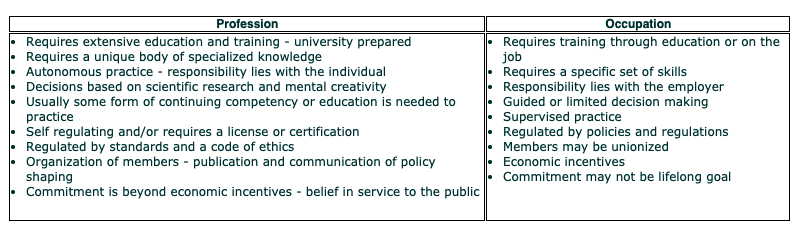 #
#
What is a Profession? #
Professionalism is not as easily defined as the term profession; it can be open to different interpretations, depending on who you ask. We know when we see it and certainly know, and feel it, when we don’t. It implies both a way of acting and being – both of which can be interpreted differently.
Think about a nurse or LPN from one of your practice experiences that you think acted like a professional. What attributes did he/she exhibit that made you think their behavior was professional? On the reverse, describe behavior that you have seen that you would not consider professional.
Professionalism is difficult to measure but academic programs help to professionally socialize students to practices and values underlying nurses’ professional identity, as expressed through what is meaningful in their work.
As students, you are taught the “ideals” or “gold standards” of a specialized body of knowledge and you are socialized to current collaborative standards of practices: Some current standards of practices may indeed be less than ideal, but we are regulated and supported by our professional college (CLPNBC) to uphold, safe and appropriate nursing practice, which can be achieved by promoting good practice, preventing poor practice, and intervening when practice is unacceptable.
Review the standards for LPN nursing practice at: CLPNBC Professional Standards of Practice for Licensed Practical Nurses and the scope of the LPN at CLPNBC Scope of Nursing Practice.
Professional nursing organizations (e.g. CLPNBC, CLPNABC, CRNBC, CNA) are instrumental in shaping nursing practice by developing standards of practice, education, ethical conduct and continuing competence. Unions, although primarily concerned with the development of legally binding agreements that regulate salaries, working conditions and other contract negotiations, also advocate for health and nursing policy related to scope of nursing practice. Professional organizations and unions have some common goals such as the welfare of members, improvement of working conditions and concern for professional ethics.
- From your clinical or educational experience, identify and select an issue that concerns you and that you think requires a new or revised policy. Post it on the discussion board.
- As you read the concerns of your colleagues – propose a change/solution to the issue and post it on the discussion board.
Professions possess certain structural and attitudinal attributes that set them apart from other occupations. Professional attitudes and behaviors develop through professional socialization – a process by which an individual will acquire the values and attitudes, interests, skills and knowledge – become a part of the culture – into the group of which they are, or seek to become a part of.
Girard, N. (2005). Are you a professional?. AORN Journal. 81(3), 487-8.
Perioperative nurses have often been scrutinized by others in health care (including other nurses) who have not considered the OR to be a place for professional nurses. Do you agree with Girard’s reasons for why perioperative nursing is considered less professional than other nursing specialties? Are we professionals? Do we present a professional front?
She suggests that one of the characteristics of a profession is that its members continually engage in ongoing learning. “Critical refection can be considered an intrinsic process that stimulates an individual to question ingrained perceptions about interpretation of and response to various situations and to question such examination by others.”
Girard recommends that we analyze our attitudes, practice ethics, roles and appearance and ask ourselves the following questions:
- Do I have a personal code of nursing ethics and behavior?
- Do I consistently act as a professional?
- Do I positively defend nursing and speak of being a nurse proudly?
- Do I lead by example, so others can follow?
- Do I assess the situations that I am in to ensure that I am practicing within my professional scope? Do I take direction from and collaborate with the appropriate individuals?
- Am I a mentor and do I share professional knowledge?
- Do I always use a surgical conscience, regardless of who is watching, or even, if no one is watching?
- Do I work to my highest potential?
- Am I a contributing representative member of my staff, profession, community and society as a whole?
- Do I strive for personal and professional growth and development?
- Do I set personal professional goals and accomplish them?
- Do I belong and participate in any professional organizations?
We have discussed some of the major elements that make nursing a profession:
- Philosophy
- Body of Knowledge
- Leaders
- Guidelines for behavior – ethics, guidelines, codes, oaths, belief statements
- Admission requirements – certification, requirement for ongoing education, testing, evaluation for admission and maintaining membership.
Summary #
Professionalism encompasses both attitude and behavior. It includes knowing how to do your job, demonstrating a willingness to learn, cooperating with others, demonstrating respect and living up to commitments. Nurses, and our knowledge, advocate for patients and ensure that health and nursing polices promote quality patient care, wherever we practice.
The profession of perioperative nursing has come a long way. Today, we face many challenges: a chronic shortage of registered nurses and licensed practical nurses, due mostly to an aging nursing population and the ability to attract and retain nurses to the profession. As students, you have embarked on an exciting journey and you are a critical force in ensuring the future of perioperative nursing. You will, after climbing up many peaks and down many valleys, possess the knowledge, critical thinking and clinical expertise to validate perioperative nursing as a profession.
Teamwork and Communication #
Learning Objectives #
At the end of the unit the student will be able to:
- List the key components and concepts of a team and how they relate to the OR
- Describe the different attributes between an effective and ineffective team
- Discuss some of the issues or challenges that affect communication in the OR
- Describe the barriers to good communication
- Describe how to deal with rude, demanding, and unreasonable behavior in the OR
- Describe some of the sources of conflict in the OR and the strategies of conflict resolution
- ORNAC: Section 3: Patient Safety – Nursing Documentation and Electronic Health Records.
- Review content from navigational links in the right hand column.
- Complete the style inventories on the following websites and be prepared to discuss if you agree or disagree of the assessments of yourself:
- What kind of communicator are you? To find out complete – Communications Style Inventory (taken from the Ocean Coast College – California – website).
- Go to the following website and review only the University of BC Faculty of Graduate Studies – graduate pathway to success website – “Conflict Resolution” section from the management skills section.
- To determine which of the 5 conflict management styles you are go to the Conflict Management Questionnaire and complete the survey (taken from the University of Arizona College of Engineering website).
The Concept of Teamwork #
I know all of you have been part of a team at one time or another; it is in fact the basis of licensed practical nursing – to collaborate with the registered nurses in the planning the care of your patients. On your current unit of work, I’m sure you and your colleagues work as a team to deliver care to your patients. The concept of teamwork is not new to any of us. In fact, we probably do it without giving it much thought. We have included communication within this unit, as it is such an integral part of teamwork that one cannot exist without the other.
The Operating Room is a place that requires a great deal of teamwork to make the patient’s experience successful. Let us begin by discussing the difference between groups and teams.
A group is defined as a number of individuals or things placed, assembled or acting together. They may have common characteristics or interests.
A team, however, is a number of persons associated together in a specific work or activity. A team has defined goals, objectives and ongoing relationships and they are focused on accomplishing a task.
Not every group is a team and not every team is effective.
When we think of teams, most often we think of them as being interdependent. This means that no significant task can be accomplished without the help of all team members. Team members typically specialize in different tasks; but the team’s success is completely dependent on each member. This interdependent team work style, more so than others, characterizes the perioperative team.
Teams can also be independent. Every person basically performs the same function and the performance of one team member has no direct effect on the next member. They may be able to help each other by offering advice or providing moral support, or by helping in some way in the background, but each individual’s success is primarily due to their own efforts. This team would be comparable to the registered nurse on the surgical unit.
There are other types of teams; virtual teams consisting of members joined electronically; and project teams used only for a defined period of time and for a separate, concretely definable purpose. We will focus on the interdependent team.
Working together successfully in a fast-paced, tense area such as the operation room requires us to understand some key concepts.
CONCEPT ONE IS COMMUNICATION. It is important that each team member understands how to conduct interpersonal relationships with their peers in thoughtful, supportive and meaningful ways. It requires that members must resolve conflicts among themselves and to do so in ways that enhance rather than inhibit their working together. It is critically important that team members learn how to state openly what is on their minds and that they be responsive and respectful as other members of the team do the same. Thus, be able to give and receive feedback constructively. These guidelines will help you give feedback successfully.
Guidelines For Giving Positive Feedback
- Clarity—Be clear about what you want to say.
- Emphasize the positive not the negative
- Be specific—Avoid general comments and clarify pronouns such as “it,” “that,” etc.
- Generalizations—Notice terms such as “all,” “never,” “always,” etc., and try to be more specific—often these words are arbitrary limits on behavior.
- Focus on the behavior rather than the person.
- Refer to behavior that can be changed.
- Be descriptive rather than evaluative.
- Own the feedback—Use ‘I’ statements.
- Be very careful with advice—People rarely struggle with an issue because of the lack of some specific piece of information; often, it is more useful to help the person come to a better understanding of their issue, how it developed, and how they can identify actions to address the issue more effectively.
In addition, team members must be able to trust that they will receive what they need while being able to count on one another to complete tasks related to team functioning and outcomes. To communicate effectively people must be willing to confront issues and to openly express their ideas and feelings. In nursing, constructive confrontation has not been a well used skill.
CONCEPT TWO is a sense of mission or purpose that is clearly understood and agreed to by all.
Willingness to work together or cooperation is CONCEPT THREE. Merely working in an operating room together does not constitute a team. You may possibly be successful in completing the task at hand which is likely getting through the surgical procedure, but without technical and interpersonal coordination and emotional investment you are not a true team.
Commitment is essential and is CONCEPT FOUR. Ideally, all members involved in any undertaking are passionate about and dedicated to the goal or the completion of the undertaking. It is possible to teach almost anyone the technical aspects of what needs to be done in most patient care settings. It is far more difficult to teach people to love what they do or to care about the patients and their families.
Issues Facing Teams #
There are many issues that all teams face therefore, it must overcome to be truly successful.
Participation is essential. Most of us want to be valued and recognized by others. We want to have some part in the decision making and feel they have some power and influence. People who feel they are a part of this dynamic process cooperate more, work harder and more effectively and bring enthusiasm to the team (more on this in the next section). Conversely, when one feels they have nothing to add or no opportunity to have their voice heard, they withdraw, work alone or daydream. This behavior creates conflict and division in the team and interferes with the smooth running of the unit.
Power and control is closely interwoven into the equation. Everybody wants enough power and influence to meet their immediate needs and to feel they are in control of the environment that surrounds them. If an individual has no control over these basic things they loose self-esteem and try to compensate in some way, which most often is not productive to a smoothly functioning team.
Appreciation for individual skills
Every individual needs to feel as though their skills and contributions are needed and valued and that they are respected for what they have to offer. Everyone has weaknesses. It is counter productive to focus on these; rather pay attention to people’s strengths, specifically emphasizing and acknowledging what people do well. Rather than trying to correct what we see as imperfections, channel your energies into appreciating people for all the remarkable things they are.
Giving people praise or the credit they are due is not easy for most people to do. The following guidelines may help you acknowledge others.
Guidelines for acknowledgment
- Acknowledgment must be specific—the actual behavior or action that is appreciated must be identified
- Acknowledgment must be eye to eye, not a comment as you are running down the hall to do something else. A written acknowledgment is equal to eye to eye.
- Acknowledgment must be sincere—from the heart
- Acknowledgment is more powerful when done in public—most people receive pleasure from public acknowledgment
- Acknowledgment must be timely—the less time that elapses between the action and the acknowledgment the more powerful the effect.
Group Agreements
A well functioning team will have agreed on the ground rules of their behavior towards one another. Rules such as being supportive in speech and actions towards your colleagues, keeping agreements, clear communication, agreeing upon goals, respectfulness go along way in enhancing your team’s ability to work cohesively. When there are no rules, people may feel they have permission to behave in any manner they choose toward one another including angry, hurtful, acting-out behavior.
Trust
Trust is a key component of not only good teamwork, thus far almost all successful relationships. An individual must know that they will not be deliberately or accidentally, consciously or unconsciously taken unfair advantage of. Trust is probably the most delicate aspect within relationships and is influenced far more by actions than by words. What people do is much more powerful than what they say. Unfortunately, trust is a fragile thread that can be severed by one act and once destroyed, it is more difficult to re-establish than its initial creation.
Teams function at varying levels of effectiveness. Truly effective teams are ones in which people work together to produce extraordinary results that could not have been achieved by any one individual. This phenomenon is called synergy. To consistently create synergy there are some basic rules to follow.
Purpose
One — Establish a clear purpose. Each member of the team must understand the reason they are together and determine what they want to accomplish. Teams function best when the members can not only tell others about their purpose but also define and standardize succinctly the meaning and the value of this purpose. This may be a difficult one as you embark into a new area of practice in the perioperative setting; in terms of establishing the scope of the licensed practical nurse and practicing within it.
Listen actively
Listening actively—means one is completely focused on and tuned into the words, posture and tone of voice of the individual who is speaking. It especially means listening without judgment. It does not mean developing a defensive response or argument in your head while the other person is still speaking.
Be Compassionate
Compassion is defined as feeling sorry for the sufferings or trouble of another or others, accompanied by the urge to help. When applied to a team situation, that definition could be interpreted as listening from a caring perspective; one that is focused on understanding the viewpoint of the other person rather than insisting on the “rightness” of one’s own point of view.
Tell the truth
To tell the truth means to speak clearly to personal points and perspectives while acknowledging that they are merely personal perspectives.
Be Flexible
No one person has all the right answers. Therefore, it is important to acknowledge that each person has something to contribute and must be heard. Flexibility reflects a willingness to hear and accept anothers’ point of view. This quality allows us to use anothers’ ideas to tackle a problem in a different but equally effective way.
Commit to Resolution
This is a commitment of all team members to listen to differing perspectives, identify the differences and creatively seek solutions to resolve the areas of differences. All parties need to feel their point of view has been heard and that they agree to the resolution made. Commitment to resolution differs from compromise in that in compromise there is a relinquishing of a significant portion of what was desired. Often compromise leaves the involved parties with negative feeling about the process, the outcome and even themselves.
In conclusion, a team cannot be truly effective when one team member becomes the self-proclaimed expert, nor when other members refuse to speak. Each team member has good ideas and these need to be shared. The challenge each person faces is to push through discomfort levels and become full participants in problem identification and resolution for the overall benefit of the team goal or objective.
Decision Making in the Perioperative Setting #
It is in inherent in the scope and nature of the LPN to function within an interprofessional collaborative environment. In the perioperative setting there are many professionals involved in the decisions regarding patient care – it is truly a team effort. There is a constant partnership between professional groups that make the operating room such a unique place to work; there is a blending together of different professional cultures, sharing skills and knowledge, and a sense of working together towards a common goal of quality patient care. All groups of professionals are important in this decision making process regarding the patient’s care.
The physician – surgeon and/or anesthesiologist – make certain decisions regarding the patient’s care in regards to the operative procedure and they work collaboratively with the perioperative nurses on the overall plan of care. As in any hospital setting, the registered nurse and the LPN will function within their scope of practice, and will collaborate on a plan of nursing care, based on a detailed patient assessment.
On any one day in the operating room a variety of patients will present, some of them stable and some of them not. They may present for surgery with no underlying medical concerns or they may have many. The nature of undergoing an anesthetic and/or surgical procedure can readily alter a patient’s level of stability and complexity. Some centers will deal with patients who have sustained a traumatic injury or multiple injuries.
The patient about to undergo a surgical procedure may not always be considered to be a stable non-complex patient.
This requires the LPN to constantly assess their level of involvement with any one particular patient – or more specifically – knowing what role to take and when to seek direction. The LPN works together with the registered nurse to decide which of the two roles – circulating or scrub – would be the most appropriate for any given patient (see next section for more detail regarding the roles).
According to the CLPNBC Baseline-Competencies for Licensed Practical Nurses’ Professional Practice (February 2009), “Practice decision-making is context-specific and changes according to client and practice-setting circumstances” (p. 18). Refer to the CLPNBC guidelines (Appendix A – A Guide to Decision Making) for the novice LPN – and in the operating room this transition to an expert level of practice (for both the RN and LPN) can take some time. The level of a professional’s experience will never supersede their legal scope of practice.
If you are ever in a situation where you feel that the patient’s condition has changed or the plan of care is outside your scope – some questions to ask yourself are:
- “Has the predictability of the client’s condition been established by a person with the ability to make that determination. If not, have I consulted with a colleague to ensure that this is an appropriate client assignment?
- Is the assessment complete (i.e. head to toe assessment of patient’s position on the operating room table)? Must I consult with a more experienced colleague or an interdisciplinary team member?
- Based on the assessment, what are the possible options of care? Do I know what the research indicates about each option, or do I have to inquire about this? What are the indications and contraindications for each option?
- Am I satisfied that the proposed nursing interventions are appropriate for the client, given the particular circumstances and the range of alternative options available?
- Do I have the authority to perform the proposed nursing interventions?
- Am I competent to perform the proposed nursing interventions
- Has the nursing care provided achieved the desired outcome(s)?”
If the answer to any of the above questions is no, then it is your responsibility to seek direction or accept direction from the appropriate person.
Role of the Perioperative Nurse #
Learning Objectives #
At the end of the unit the student will be able to:
- Define perioperative nursing
- Define perioperative nursing as set down by the ORNAC standards, guidelines and position statements for perioperative registered nurses (RN) and licensed practical nurses (LPN)
- Describe the role of the scrub nurse
- Define the differences between the role of the RN and the LPN in the scrub nurse role
- Describe the role of the circulating nurse
- Define the differences between the role of the RN and the LPN in the circulating nurse role
- Describe the role of the other health care professionals in the perioperative setting
- Alexander’s Care of the Patient in Surgery: Review Overview of Perioperative Nursing Practice in Chapter
- Canadian Council for Practical Nurse Regulators (CCPNR) – Standards of Practice & Competencies for Perioperative Licensed Practical Nurses – Part Three – Competencies for Perioperative Licensed Practical Nurses.
Now that you have read about perioperative nursing:
- Review the content from the navigational links in the right hand column.
- Review the video of a scrub & circulating nurse in a realistic setting, as they perform one set of their duties – preparation of the operating room for surgery (a laparotomy). Download the notes from page 4.1 – The role of the scrub and_circulating nurse to review as you watch.
The Perioperative Team #
The perioperative period encompasses the time surrounding the operative procedure. The phases are:
Preoperative
- From the time a surgical intervention has been planned to the time the patient is taken to the operative suite
Intraoperative
- From the time the patient is taken to the operative suite to the time the patient is ready for transport out of the OR
Postoperative
- From the conclusion of the surgical intervention through the recovery phase and resolution of any rehab activities
#
Perioperative Team #
The perioperative team may include:
- Surgeon – responsible for the overall care of the patient preoperatively, intraoperatively and postoperatively. The surgeon will be the only member of the team who has a previous history with the patient and knows the patient’s personal history. They are the one who has made the decision to operate on the patient. The surgeon will perform the operation with an assistant – this will be either a resident or fellow (a physician training in a specific surgical specialty) or a medical practictioner trained in surgical assisting.
- Anesthesiologist – responsible for providing pain relief in the form of an anesthetic during the procedure and for maintaining pain relief in the immediate phase of postoperative recovery (sometimes on the surgical floor as well). The anesthesiologist may also have resident physcians assisting them. The anesthesiologist is responsible for the physiological well being of the patient and makes decisions regarding whether the patient is fit for surgery and if they are hemodynamically stable during all phases of the surgical procedure. The patient may visit the anesthesiologist prior to the surgery to determine their surgical risk, make any corrective actions to lower their risk, and to formulate a plan of care to minimize any risks during the all phases of the surgical procedure.
- Nursing personal – The nursing personal consists of registered nurses and licensed practical nurses. They take on the roles of the circulating and scrub nurse (see the next section for a more detailed description of their role). Nursing personnel will often meet the patient for the first time in the preoperative area; so their plan of care will come from their intial assessment, from previous experience of similar operative procedures and from information gathered from the surgeon and anesthesiologist. The nursing care plan will be a collaborative effort between these three groups of individuals.
- Other auxiliary members of the perioperative team may include:
– Anesthetic technicians – specialized respiratory therapists who assist the anesthesiologist (and nurses) with difficult airways
– Perfusionists – assist in cardiac surgery by running the cardiopulmonary bypass machine
– Perioperative assistants (orderlies) – assist surgeons and nurses with positioning patients and other non-nursing duties
– EEG or ECG technicians – assist during operative procedures where pacemaker or brain function needs to be monitored
– X-ray technicians – assist by taking introperative x-rays
– Sterile processing department (SPD) staff – trained in the decontamination, packaging, and sterilization of instruments and supplies
– Clerks – perform the clerical work required in the operating room (i.e. booking surgeries, computer input, etc)
– Translators – assist with translating for patients who speak another language
Roles and Responsibility of the Scrub and Circulating Nurse #
The purpose of this unit is to outline the roles and responsibilities of both the scrub and circulating nurses and to visualize how the two interact throughout the perioperative period to provide safe and appropriate patient care.
The coordinated roles of the scrub person and the circulator act as a specialized team within the bigger team. The scrub nurse has most of the fun and glory as he/she plays on center court where the action is: passing the scalpel, instruments, sutures etc. However, the scrub nurse is only as good as the person who set-ups them up, the circulator or the behind the scenes person, ensuring that all parts of the surgical procedure move along efficiently.
Although many of their duties are separate from one another, a spirit of mutual cooperation is essential to keep the operating room running smoothly and efficiently. They should plan their duties and with coordinated effort, the sterile and unsterile parts of the surgical procedure move along simultaneously. Ultimately, the team serves the best interests of the patient who is most vulnerable at the time of surgery.
Have you ever had surgery? If so, do you remember anything about the team – think about what was good and what might have been bad about your experience. What do patients remember about the procedure? Usually a nurse who made them feel at ease, explained what was going to happen, and made them comfortable.
Scrub Role #
The scrub nurse may be a registered nurse or a licensed practical nurse (ORLPN) who has completed training in such technical areas as principles of sterilization, aseptic technique, instrumentation and sutures.
The scrub nurse functions within the sterile field and facilitates the operative procedure by providing instruments and supplies to the surgeon. The scrub nurse is responsible for collaborating with the surgical team to assemble supplies and to prepare and maintain the sterile field. The scrub nurse must anticipate the needs of the sterile team (For example, additional sterile supplies and/or equipment) during the surgical procedure and provide for those needs in an efficient and safe manner.
Upon completion of the procedure, the scrub nurse is responsible for the safe disposal of contaminated supplies, caring for instruments and equipment, and assisting with patient care as needed.
The scrub nurse acts as a patient advocate by:
1) Maintaining a safe and efficient environment
2) Practicing and monitoring aseptic technique
3) Performing sponge, needle and instrument counts
4) Handling and identifying specimens correctly
5) Protecting the patient’s privacy, dignity, safety, and comfort
6) Identifying emergency situations during the procedure (i.e. bleeding) and informing the circulating nurse so that they can work together to provide corrective actions
The scrub person must be able to apply basic knowledge of surgical procedures, anatomy and physiology for each patient. It is the responsibility of each team member, including the scrub person, to seek opportunities to increase his or her knowledge base with regard to changes in health care and technology.
Circulator Role #
The licensed practical nurse may also function in the circulating nurse role with adherence to the professional Standards of Practice that guides safe LPN practice. They will always function alongside a registered nurse to carry out many of the responsibilities listed below.
The circulating nurse is responsible for the nursing care of the perioperative patient, primarily during the immediate preoperative and intraoperative periods, but also in the immediate postoperative phase (until the care of the patient is transferred to the postoperative recovery room nurse).
The circulating nurse is responsible for coordinating the nursing care of the patient throughout the intraoperative period. These activities include:
1) Assessing the patient, including both physiologic and psychosocial health status
2) Formulating nursing diagnoses pertinent to the perioperative period
3) Establishing patient goals for optimal expected outcomes
4) Developing a plan of care and outlining nursing activities that will achieve these goals
5) Applying monitoring equipment
6) Assisting the anesthesiologist within their profession’s approved standards, limits and conditions
7) Implementing nursing actions, either directly or by delegating the action to a qualified team member, including:
a) Creating, maintaining and monitoring a sterile field
b) Providing equipment and supplies
c) Performing sponge, needle and instrument counts
d) Administering drugs and solutions as prescribed
8) Evaluating patient outcomes and adjusting the plan of care too reflect the current status of the patient throughout the perioperative period
The circulator incorporates teaching activities into the care of the patient and family. Knowledge deficit is a common nursing diagnosis in perioperative nursing. The circulating nurse:
1) Identifies the learning needs of the patient and/or family
2) Assesses their readiness to learn, influenced by anxiety levels and attention span
3) Provides instruction based on learning needs
4) Evaluates the effectiveness of the teaching
The circulating nurse is responsible for the documentation of all nursing activities that take place during the perioperative period. Although documentation formats and methods differ among surgical settings, there are elements common to everyone.
The preoperative checklist is started by the nurses in the patient admission area. It usually contains but is not limited to:
1) Identification of the patient
2) patient assessment data
3) verification of the presence of the consent, physician history, laboratory, ECG, x-ray and other diagnostic results
4) presence and disposition of prosthetic devices, and/or sensory aids
5) NPO status
6) allergies
7) disposition of jewelry
8) signature of persons providing patient care during the preoperative period
The operative record covers every aspect of the patient’s care during their time in the operating room. The elements include but are not limited to the following:
1) identification of persons providing patient care during the intraoperative period
2) skin condition on arrival and discharge from the surgical suite
3) positioning and devices used
4) skin prep, including solutions used
5) wound classification
6) electrosurgical unit (ESU) identification, location of the dispersive pad, and settings used during the procedure
7) other devices used—including temperature regulating devices, invasive and noninvasive monitoring devices, tourniquets, insufflators and lasers, with pertinent details regarding their use
8) administration of medications, irrigations, solutions, or blood products
9) specimens and cultures taken
10) implants, including lot numbers and other information required for tracking
11) documentation of sponge, sharp, and instruments counts
12) use of intraoperative x-rays
13) dressings and drains
14) time of discharge; method and place of transfer
15) any other significant or unusual occurrences that may affect patient outcomes
The count sheet contains a detailed account of all of the sterile items used, sponges, sharps, miscellaneous small items and instruments. Counts are performed by both the scrub and circulating nurses prior to commencement of surgery, at first layer of closure depending on the cavity entered and at skin closure. Both participants sign this sheet.
Patient advocacy is the responsibility of each member of the surgical team but is an important part of the circulating nurse’s role. The circulator has the overall responsibility for all nursing and staff activities pertaining to the patient and has gathered specific data regarding the individual needs and desires of that patient. Advocacy implies acting on behalf of another, and the circulating nurse may speak for the patient during the intraoperative period when the patient is unable to speak for themselves. Advocacy may include:
1) Protection of the patient’s privacy (i.e. maintaining confidentiality and limiting exposure during positioning, prepping, and draping)
2) Protecting the patient from infection (i.e. monitoring aseptic techniques of all team members).
3) Protecting the patient from injury (i.e. improper positioning, ensuring proper function and use of equipment)
4) Identification of spiritual and cultural/ ethnic beliefs that may include some special needs during the perioperative period (i.e. the refusal of blood products by a Jehovah’s Witness patient).
5) Communication of specific needs and desires of the patient to the other members of the surgical team; and communication of care upon transfer to the post anesthetic care unit
