Description #
To discuss the importance of pain assessment, and describe pain assessment tools used to guide the diagnosis and treatment of pain.
Learning Objectives #
At the end of this course the health care professional will be able to:
- a. Describe pain assessment principles
- b. Identify the goals of a pain assessment
- c. Understand how to complete a basic pain assessment
Introduction #
Everyone responds differently to pain and pain management treatments. It is very crucial to have knowledge of different types of pain. Previous management modules have described Pain to be either chronic or acute. Everyone of us have our own expectation regarding the experiences of pain and pain management. Therefore, Pain management must be unique to every individual and it begins with Pain Assessment. Pain Assessment is the cornerstone of pain management, which is aimed at eliminating, reducing or interfering with pain.
This learning module is designed to enhance knowledge surrounding pain assessment.
Pain Assessment #
In 1992, the American Pain society defined pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage.”
Pain is a personal feeling that is unique to every individual. It is an experience that cannot be separated from the patient’s mental state, environment and cultural background. Pain is whatever a person says it is and it exists whenever a person says it does.McCaffery, M., & Pasero, C. Pain: Clinical Manual, 2nd edition. St. Louis Mosby.1999
Interpretation, tolerance and response to pain is affected by:
- Emotional and Psychological state
- Beliefs and Values
- Upbringing
- Age
- Sex
- Social and Cultural Influences
- Attitude
- Memories of past pain experiences
- Expectation
Unrelieved pain can have enormous physiological, psychological and social impact on the patient and their families. The quality of life is disturbed due to impaired sleep, social relationships and daily functioning.
Unrelieved pain can:
- Be harmful and expensive
- Inhibit Immune System
- Cause respiratory dysfunction
- Decrease Gastrointestinal Tract
- Enhance Tumor growth
- Increase patient’s chance to have Atelectasis.
- Cause confusion
- Increase O2 demand
Patients have the right to the best pain relief treatment possible and it begins with a comprehensive assessment of the patient. If you ask about comfort/pain at each encounter with a patient, you foster the healing relationship and bond, the patient will be more willing to share how they are feeling if you ask. If you consider Pain as the 5th vital sign, it will not be missed.
This assessment can:
- Improve communication between nurse and the patient.
- Facilitate the development of a therapeutic and trusting relationship.
Pain Assessment must be performed when:
- Patient is admitted to unit/area.
- Change in patient’s condition/behavior.
- The patient say there is discomfort.
- On a routine basis during your shift.
Process #
Process of Assessment
It is far more than, simply, asking for a pain rating. Self-report is the most accurate measure of pain and pain relief, yet many clinicians are reluctant to accept and respect self-report. Old practice persists where the clinician rates a patient’s pain as different from the patient’s self report.
Initial assessment should be completed at first point of contact – on admission to an in-patient setting, and at first point of contact in ambulatory, primary care and home settings. Routinely scheduled screening for pain for all patients is a key component of pain care. In outpatient, ambulatory care, primary care and home care settings, all patients could be asked about pain at each visit. In the in-patient settings screening for the presence of pain could occur no less than every shift and more often if pain is unrelieved.
A pain assessment must be completed on admission, and when pain is reported, anticipated or suspected. Reassessment and documentation of individual responses to treatment must be completed after all interventions to treat pain. The assessment needs to encompass multidimensional parameters because of the complexities of the individual’s experience of pain. A full multidimensional assessment explores physical, psychological, social, cultural and spiritual components of pain but this is not always necessary to provide care.
Multidimensional Tool Sample
In the past week, how much has pain interfered with the normal activities of a person.
These activities are outlined below:
1. Family/Home Responsibilities:
Activities related to the home or family.
It includes chores and duties performed around the house (example: yard work) and errands or favors for other family members (example: driving the children to school).
2. Recreation:
This category includes hobbies. sports and other leisure-time activities.
3. Social Activity:
This category includes parties, theatre, concerts, dining out and other social activities that are attended with family and friends.
4. Occupation:
It refers to activities that are directly related to one’s job. This includes non-paying job as well such that, of a homemaker or volunteer worker.
5. Relationships with others (including: Sex life, intimacy and relationships).
6. Self-care:
It includes personal maintenance and independent daily living activities (example: Taking a shower, driving, getting dressed).
7. Life-support activity:
This category refers to basic life-supporting behaviours such as eating, sleeping and breathing.
Documentation #
Documentation of your Pain Assessment:
It is important to document the results of your assessment and document the patient response to the scale you have used. Documentation is the communication of the management plan and the responses to treatments. You can document in the form of the mnemonic you used to assess and note the patient score on the scale you used. Consistent use of the scale most comfortable for patient will allow for consistent responses regarding their pain which will facilitate your pain management plan changing scales, terms and practices leads to confusion for all involved.
There are many ways to record the information obtained, take a moment to consider how you might do this and what documentation tools you might use – graphic sheet, a flow sheet or the progress notes.
The assessment of a patient’s pain and comfort level should be monitored and documented q8h minimum. You must document patient’s self report of pain and document the patient’s behaviour that give an indication of pain. Some of the typical behaviour is frequent calling, resistance to position changes, restlessness, aggitation and moaning. Also, the environmental factors that have an impact on pain must be identified. Minimizing noxious stimuli, noise, music, weather, lights and smell (if possible) may make the patient more comfortable and reduce pain. Identifying and monitoring the emotional aspect of a patient is crucial to pain assessment as well.
Pain Assessment #
The first step of pain assessment is to take the history of pain. A variety of mnemonics can be used to assess the symptoms of pain.
The following table outlines some of the mnemonics that can be used are:
 #
#
Aside from these mnemonics more information must be attained, which can be done by asking these following questions:
Analgesic History: What analgesics have you tried in the past?
What do they take at home?
What was the response to their past or current medications?
Impact of Pain: How is this pain affecting their functioning and quality of sleep?
Is it delaying their recovery?
Personal perceptions about pain/analgesia: What does pain mean to this person?
What is the goal of pain management?
Pain Assessment Tools #
Some conventional Pain assessment tools are:
One-dimensional Assessment rates pain numerically, linear or with descriptive words indicating severity. This assessment is beneficial to treating Acute pain.
Some test examples are:
NRS (Numerical rating scale): Measures a patient’s pain intensity by assigning a number to their pain level. It is based on a scale of 0 to 10 where zero represents no pain and ten represents the worst imaginable pain.
Sample:
No Pain 0—1—2—3—4—5—6—7—8—9—10 Worst Pain Possible
Advantages:
- Quick, simple to use, score and document,
- Can be used verbally or visually
- Easily translated into other languages
- Can be easily included in a flow sheet or graphic record.
- Comparison of scores can be easily visualized
- Can offer some consistency documentation within a facility or area
- Can detect response to treatments
Disadvantages:
- Patient must clearly understand that the scale is a representation of intensity
- May not be reliable with the aged, very young, cognitively impaired
- May be difficulty to use during severe pain
VAS (Visual Analog Scale): A simple measurement tool that tries to measure pain. It consists of a 10cm line with one end labeled as “No Pain” and the end other end as “Worst Pain Possible”. Pain rating is marked on this 10cm line by the patient.
Sample:
No Pain I—————————————————————————————–I Worst Pain Possible
Advantages:
- Quick, simple to use, score and document,
- Can be used verbally or visually
- Easily translated into other languages
- Can be easily included in a flow sheet or graphic record.
- Comparison of scores can be easily visualized
- Could be correlated to numeric scale
- Can offer some consistency documentation within a facility or area
- Can detect response to treatments
Disadvantages:
- May not be reliable with the aged, very young, cognitively impaired
- May be difficulty to use during severe pain
Faces pain scale: This pain scale uses the patient’s facial expression to measure the severity of pain. A 6-cartoon faces diagram (shown below) is used to rate the pain.
Sample:
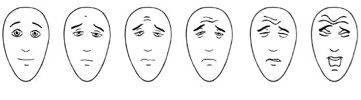
No Pain Worst Pain Possible
Free Pain Scale – Revised ©2001. IASP. www.painsourcebook.ca Hicks CL, von Baeyer CL, Soaffird P, van Korlaar I, Goodenought (2001)
Advantage:
- Simple, quick, easy to score, no reading or verbal skills required.
Disadvantages:
- Can be seen as measuring mood rather than pain
- Sad or crying faces may not be universal across cultures
Thermometer:
Sample:
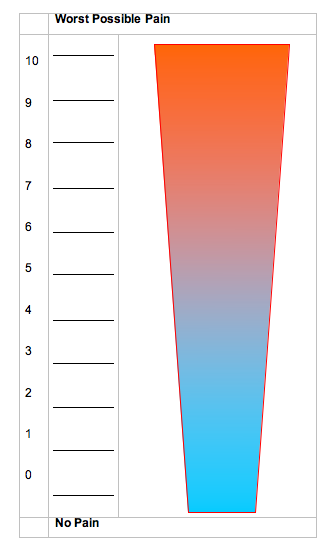
This tool is excellent for patients who cognitive deficits are moderate to severe or who have difficulty communicating verbally.
Multi-dimensional Assessment: Explores the person’s pain and experience of pain to varying degrees. It is not just a rating of severity but it takes a look at the impact of pain in various aspects of life. This assessment is beneficial to treating Chronic pain.
Some test examples are:
Brief Pain Inventory: consists of multiple questions regarding pain and how it impairs function, administration verbal and visual.
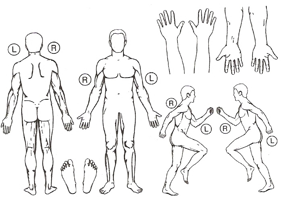
Sample:

Jovey, R., Boulanger A., and Clark A. et al. (2008). Managing Pain The Canadian Healthcare Professional’s Reference. Baker Edwards Consulting Inc.
Advantages:
- Addresses multi-dimensionality of pain experience
- Standardized reporting tool
- Can be translated to other languages
- Assesses location, intensity and pattern
- Reports medications, pain relief, patient beliefs, and effect on quality of life
Disadvantages:
- Requires cognitive skills to complete
McGill Questionnaire (Long and Short Form): This questionnaire uses multiple questions and is administered in a verbal/visual format. The short questionnaire measures the intensity, sensory and affective dimensions of Pain. The long form measures the location, pattern of pain over time along with the intensity, sensory and affective dimension of pain.
Sample:
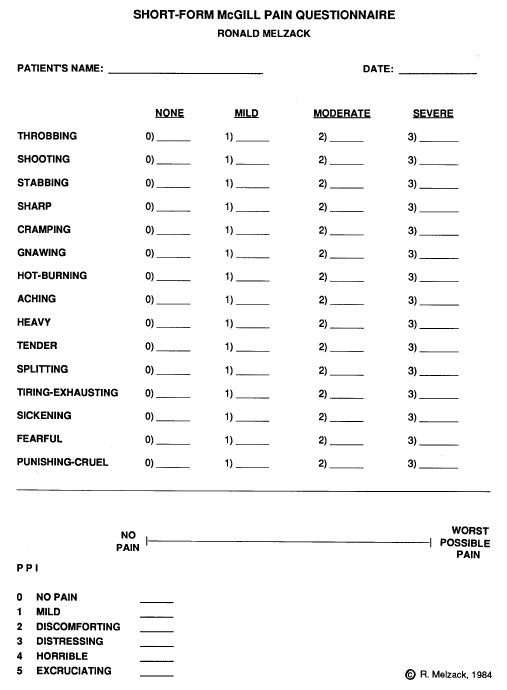
http://prc.coh.org/pdf/McGill%20Short-Form%20Pain%20Questionnaire.pdf
Advantages:
- Descriptors are provided
- Short form takes 2-5 minutes to complete
- Has wide spread use in chronic pain.
Disadvantages:
- Long form takes 30 minutes or more.
- Some descriptor words relate to pain intensity.
- Requires cognitive skills and language skills (some complex vocabulary is used).
- Does not include impaired functioning or remaining function.
- Not multicultural in terms of language meanings.
Neuropathic Pain #
Neuropathic Pain is the result of neural injury, inflammation or irritation in the peripheral nervous system or central nervous system. It is frequently described as a burning, shooting or stabbing sensation and the affected area is hypersensitive. Another characteristic of neuropathic pain is Allodynia. It persists long after injury and maybe due to abnormal pain transmission. Neuropathic pain is frequently chronic, and does not respond well to opioids, but other drugs such as anti-seizure and antidepressant medications are very effective. Mostly, Neuropathic pain is partially reversible if treated with proper treatment.
There are specific tools for neuropathic pain assessment. Some of these tools are:
DN4: is a questionnaire tool used when a physician suspects of Neuropathic pain. Each question has a simple “Yes” or “No” answer and focuses on sensation of burning, cold, electric shook, tingling, pin/needles and numbness. The physical examination portion focuses on sensitive to touch, pin prick and gentle brushing.
There are four questions, with a total of 10 items to check off:
- The clinician asks the patient the questions and fills in the questionnaire
- The answer choices are a simple yes or no.
- At the end, the clinician adds up the score, counting 1 for each yes and 0 for each no.
- The sum obtained gives the patients score, out of 10
Sample:
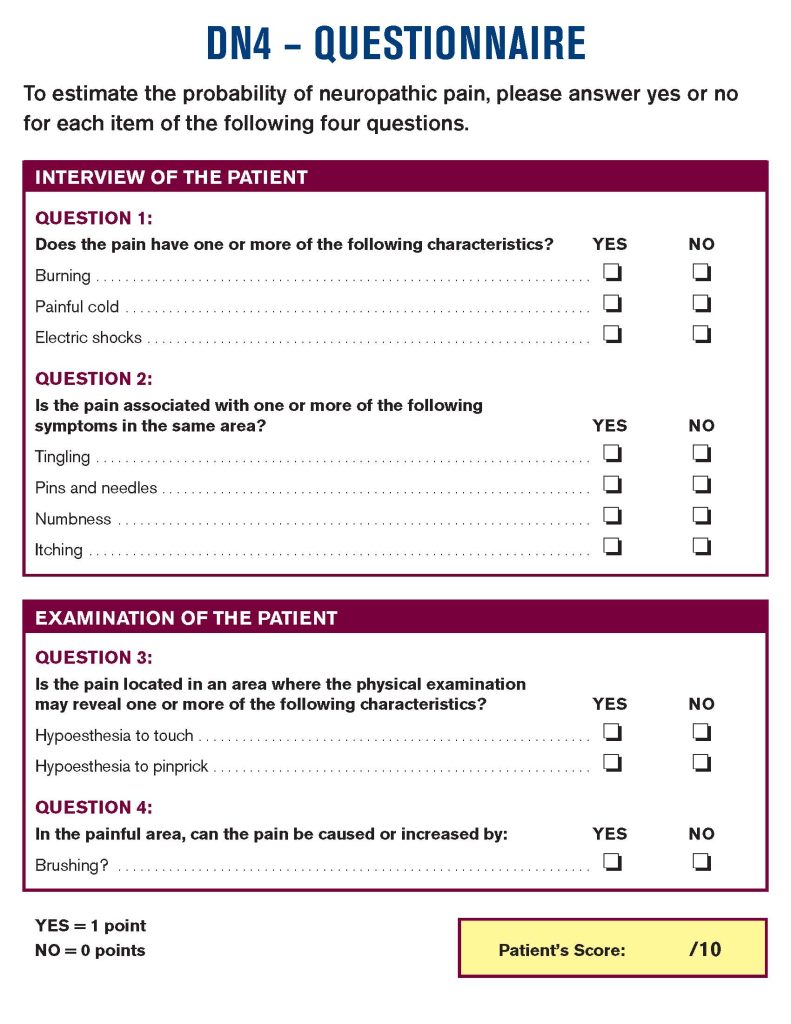
http://www.dn4.ca/local/files/pdf/en/questionnaire.pdf.html
Advantage:
- Simple, 4 questions with 2 examinations
Disadvantage:
- Requires examination and physical testing.
NeP Short Form: asks 3 questions regarding tingling, numbness and Allodynia. The answers are rated on a 0-100 scale. There is a value to multiple by for each answer then added and subtracted by 1.302. If answer equal to or greater than zero it is positive for Neuropathic pain (NeP).
Sample:
The Clinical Journal of Pain 19: 315-316 © 2003 Lippincott Williams & Wilkins, Inc., Philadelphia
Calculation sample: Tingling 0-100 x 0.015, Numbness 0-100 x 0.017, Allodynia 0-100 x 0.011, add all of the scores and then subtract it by 1.302. If the value is equal to or greater than zero, it is positive for neuropathic pain.
Advantages:
- 3 questions.
- Answers are rated on 0-100 scale.
Disadvantages:
- Requires cognitive skills and language skills (complex vocabulary is used).
- Professional must obtain result through calculating the numeric responses.
Additional Pain Assessment Tools #
Opioid Risk Tool: Clinical Form
The screening and addiction risk stratification tool is meant to be completed by the physician – not the patient. However. it can be completed by the patient if the scoring is removed from the form.
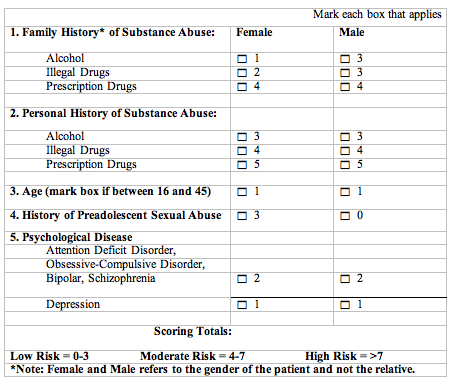
Webster LW. Pain Medicine 2005; 6(6): 432-442
Jovey, R., Boulanger A., and Clark A. et al.(2008). Managing Pain The Canadian Healthcare Professional’s Reference. Baker Edwards Consulting Inc.
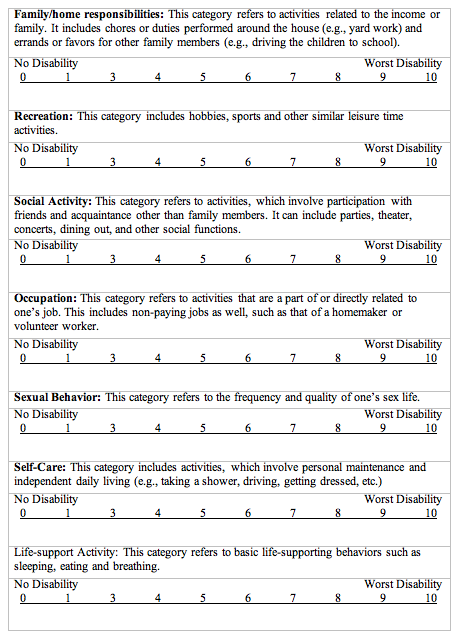
Pain Disability Index [PDI]:
The rating scales below are designed to measure the degree to which aspects of your life are disrupted by chronic pain. In other words, we would like to know how much your pain is preventing you from doing what you would normally do, or from doing it as well as you normally would. Respond to each category by indicating the overall impact of pain in your life, not just wen the pain is at its worst.
For each of the 7 categories of life activity listed, please circle the number on the scale, which describes the level of disability you typically experience. A score of 0 means no disability at all, and a score of 10 signifies that all of the activities in which you would normally be involved have been totally disrupted or prevented by your pain.
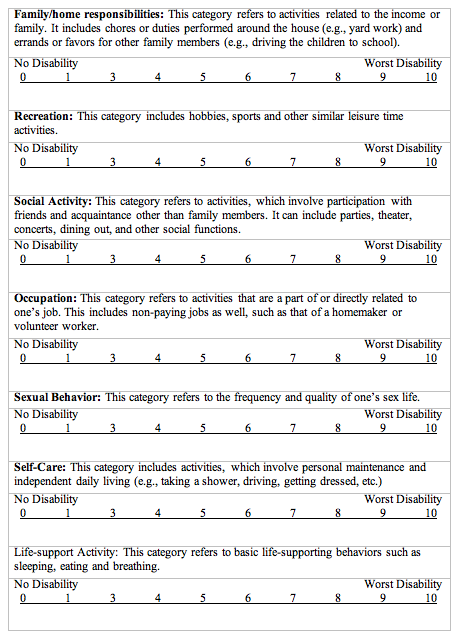
Jovey, R., Boulanger A., and Clark A. et al.(2008). Managing Pain The Canadian Healthcare Professional’s Reference. Baker Edwards Consulting Inc.
Patient Teaching #
Teaching patients about pain and pain management is a crucial aspect of providing care.
A teaching plan must include:
- The patient’s family, if possible.
- Instructions on how to use different pain scales.
- Encourage patient to report pain.
- Discussion on the misconceptions of addiction, fear of drug dependence and fear of being judged in a negative way. misconceptions as needed such as fear of addiction, dependence, or being judged in a variety of ways.
- Emphasizes on the need to request medication to stop pain before it becomes severe.
- How to take comfort measures to reduce pain and increase comfort level. some examples are repositioning, splinting area, relaxation techniques and activity modification.
- Safety measures such as use of side-rails following administration of medication.
Summary #
The most common reason for lack of pain relief in hospital is failure to assess pain. Comprehensive assessment is the first step to learn about another’s pain, establish an effective individualized plan, and evaluate responses to pain treatment.
Assessment is central to quality pain management. Asking questions, involving the patient, observing, checking physical parameters are all important components of a pain assessment. While using a scale, such as 0-10, does provide relevant important information, this in itself is not a full pain assessment. Additionally, all assessment should involve reassessment after any intervention or action is implemented to relieve pain.
Remember the steps to quality pain management:
Ask the patient
Assess regularly
Believe the patient
Choose comfort options
Deliver interventions
Document
Empower patients
Enable them to control their course as much as possible
Case Study :
In this module we will be following a patient during her stay in hospital. You will learn more about her as you read along.
Mrs D is a 56 year old woman who tripped at home and fell down the stairs. She injured her left rib cage and fractured her left hip. She was admitted through the Emergency department and had a left hip replacement yesterday. There was no head injury or other injuries detected. You meet her at the start of your shift and she tells you she has pain.
Activity 1
What information would you like to learn about Mrs. D?
She is a 56 year old married woman living with her extended family in a house. She is the mother of 2 grown children who are in university. She is usually healthy except for some arthritis. Her chest X-ray shows no fractures, her left hip was replaced early yesterday. Her post operative orders for pain are:
Tylenol 975 mg TID
Naprosyn 500 mg BID
Oxycodone 5 mg Q6h PRN
Her MAR shows that she has had Oxycodone 5 mg Q6H since returning from the OR yesterday morning. She has been up with physiotherapy to stand once but complained of severe pain.
What else do you want to know about her pain?
You complete a pain assessment and learn she has 3 areas of discomfort
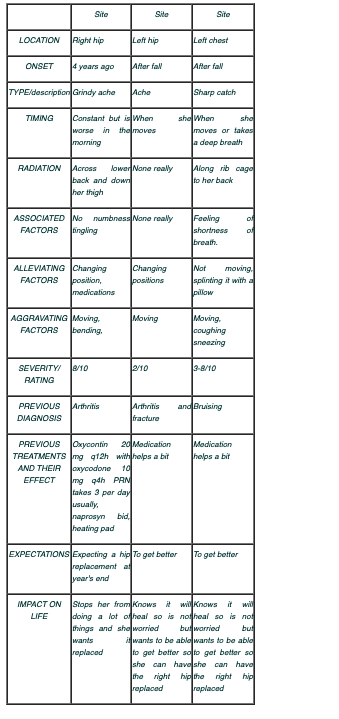
What else do you want to know? What are your next steps?
Activity 2
Next Step : Examination
Physical Examination:
You examine Mrs. and find a woman looking her stated age, alert and oriented but has a furrowed brow and is hugging a pillow to her left side. Her skin is pink warm and dry, vital signs are BP 122/84 P 84 regular RR 12 and shallow. You notice that she has diffuse bruising over the left lower chest, no subcutaneous emphysema, no obvious deformity and her breath sounds are clear to the bases. She has a clean dry incision left lateral thigh no redness, swelling or exudate, non tender to the touch. Her right hip and back are non tender to touch but she moves stiffly in the bed and tells you she feels it “grinding inside” and as if there is a “prickle” inside. Her feet are pink warm and dry with palpable pulses at the DP and PT, cap refill of her toenails is less than 3 seconds.
What is your plan of action?
Activity 3
Documentation
Case Study: In this module we have been following Mrs. D. and now have gathered information and need to make a plan of care and document the plan so that others will know what we have learned. The following is an example only, each area and hospital has guidelines for documentation as well as specific tools for recording information in the Legal Heath Record which are to be used. This example is for practice and demonstration and should not replace standardized tools.
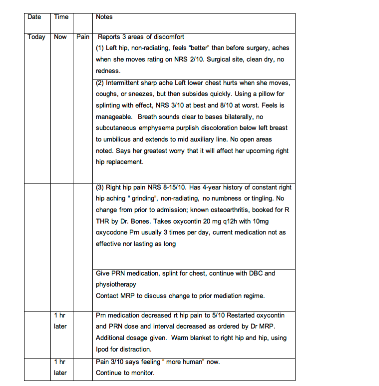
#
References:
- Ellis, J.A., Blouin, R., Lockett,J., Patient-controlled analgesia Optimizing the Experience. Clinical Nursing Research, Vol. 8, No.3, August 1999, p 283-294.
- Faries, J., Controlling Pain: Treating Oversedation and Respiratory Depression. Nursing 1998, December.
- Faries, J., Controlling Pain: Making a Smooth Switch from IV Analgesia. Nursing 1998, July.
- Jones,S.K., An Algorithm for Train-of-four Monitoring in Patients Receiving Continuous Neuromuscular Blocking Agents. Dimensions of Critical Care Nursing, March/April 2003, Vol. 22, No. 2, p 50-57.
- Jovey, R ( ED) Managing Pain: The Canadian Healthcare Professional’s Reference. The Canadian Pain Society: Toronto. 2004.
- McCaffery, M., & Pasero, C. Pain: Clinical Manual, 2nd ed. St Louis: Mosby. 1999
- McCaffery,M., Robinson, E.S., Your Patient is in Pain – Here’s how you Respond. Nursing 2002, October, Vol. 32., N0. 10, p 36-45
- Morphett,S., Nerve Blocks for Anesthesia and analgesia of the Lower Limb – A Practical guide: Femoral, Lumbar, Plexus, Sciatic. Retrieved from www.nda.ox.ac.uk April 2005.
- Raj, P., Schwiers, J., Nerve blocks: are they useful and significant in the management of pain patients? Pain Reviews, 1999, 6:193-201.
- Stannard, C. & Booth,S Pain 2nd Edition Churchill Livingstone:Toronto. 2004Jovey, R (ED) Managing Pain: The Canadian Healthcare Professional’s Reference. The Canadian Pain Society: Toronto. 2004.
