Description #
This unit will describe the correct administration, scoring and interpretation of the Numeric Pain Rating Scale (NPRS) for TJA patients.
Learning Objectives #
By the end of this unit, the learner will be able to perform the following tasks for TJA patients:
– Administer the Numeric Pain Rating Scale (NPRS)
– Score the Numeric Pain Rating Scale (NPRS)
– Interpret the Numeric Pain Rating Scale (NPRS)
What is this test? #
What is the Numeric Pain Rating Scale? #
The Numeric Pain Rating Scale (NPRS) is a valid3,4 and reliable1,2 measure for assessing THA and TKA patients and falls within the WHO’s ICF domain of Body Function/Structure9 (Figure 1). The NPRS measures a single dimension of joint-specific or global pain intensity at rest or with activity1. In addition, it can be administered quickly requiring a total of approximately 1 minute to complete and score.
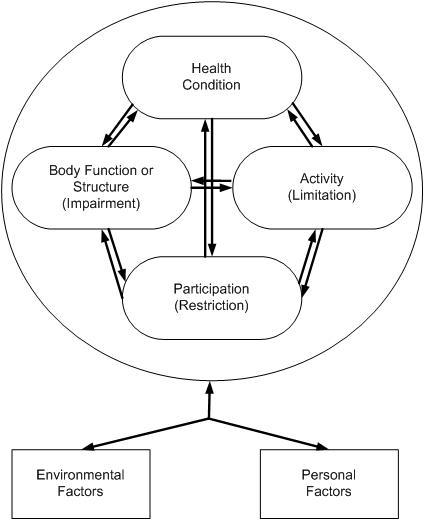
Figure 1. The International Classification of Functioning, Disability and Health (ICF) Conceptual Model. Taken from Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. Figure 2-110.
When do I use it? #
When do I use the Numeric Pain Rating Scale? #
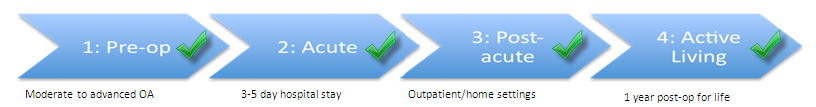
The Numeric Pain Rating Scale (NPRS) can be used in all the phases along the TJA Continuum of Care. Indeed, as you can see in Figure 2, the NPRS is recommended for use in the Pre-Operative, Acute, Post-Acute, and Active Living phases of the TJA continuum. Health professionals can therefore use this outcome measure to monitor change in the patient’s status as he or she moves through all the phases of care.
Figure 2. The phases along the TJA Continuum of Care for which the NPRS is recommended.
CLINICAL TIPS!
- Both the NPRS and the Visual Analogue Scale (VAS) are recommended outcome measures for pain. But which one is more appropriate? That depends on the patient, the therapist and the equipment available.
- For example, if your patient has difficulty using numbers to describe their pain, the VAS would be the better choice. Similarly, if the therapist did not have a ruler for measurement, the NPRS scale would be better.
Equipment needed? #
What equipment is used to complete the Numeric Pain Rating Scale? #
For the patient to complete the Numeric Pain Rating Scale (NPRS) with a patient, the following equipment is required:
- A paper copy of the NPRS
- Pen
Figure 3. The Numeric Pain Rating Scale
 #
#
CLINICAL TIPS!
- Whenever you are using the NPRS, you may wish to note what pain medications the patient is taking since pain medications can affect the patient’s NPRS score!
How do I do it? #
How do I administer the Numeric Pain Rating Scale? #
It is simple to administer the Numeric Pain Rating Scale (NPRS) – instruct the patient to circle a number on the line indicating how much pain they are currently feeling either during rest or activity.
How do I score it? #
How do I score the Numeric Pain Rating Scale? #
Scoring the Numeric Pain Rating Scale (NPRS) is easy to do.
- Have the patient select a number between zero (no pain) and ten (worst pain possible) to rate their current pain intensity at rest or with activity.
- Record the value reported by the patient
Figure 3. The Numeric Pain Rating Scale (NPRS)
 #
#
What does it mean? #
How do I interpret the Numeric Pain Rating Scale? #
It is simple to interpret the Numeric Pain Rating Scale (NPRS) – the higher the score, the more intense the pain. Furthermore, did you know that TRUE CHANGE is indicated by a reduction of only 3 points in the NPRS6. It’s true! It has been established that the:
MDC is 3 points in patients with musculoskeletal problems receiving physical therapy6.
- What does this mean for my patient? It means that the change in score between test occasions must be greater than 3 points in order to reflect a true change and not just measurement error.
MCID is 30% in patients with OA or low back pain7
- What does this mean for my patient? It means that in patients with OA or with low back pain, the change in score between test occasions must be greater than or equal to 30% in order to indicate that a clinically meaningful change has occurred. To see how this is calculated, click the Examples tab on the right hand side.
MCID is 29% in patients who have undergone orthopedic surgery8
- What does this mean for my patient? It means that in patients who have undergone orthopedic surgery, the change in score between test occasions must be greater than or equal to 29% in order to indicate that a clinically meaningful change has occurred. To see how this is calculated, click the Examples tab on the right hand side.
Example 1 #
On assessment Mr. S reported that his left knee pain secondary to OA was 7/10 on the NPRS. After 6 weeks of PT intervention, Mr. S reported that his knee pain was 4/10. The MCID for patients with OA is 30%.
Has clinically meaningful change occurred?
1. Calculate the MCID
2. Calculate the change in score between test occasions
3. Compare the MCID to the change in score between test occasions
3 > 2.1
Yes, clinically meaningful change has occurred because the difference between test occasions is greater than the MCID of 30% or 2.1.
Example 2 #
You are a community PT visiting Mr. S who has had a Left TKR. Currently, Mr S. reports that his left knee pain is 9/10 on the NPRS. After 2 weeks of PT intervention, Mr. S reports that his pain is 7.5/10 on the NPRS. The MCID for patients who have had orthopedic surgery is 29%.
Has clinically meaningful change occurred?
1. Calculate the MCID
2. Calculate the change in score between test occasions
3. Compare the MCID to the change in score between test occasions
1.5 < 2.61
No, clinically meaningful change has not occurred because the difference between test occasions is less than the MCID of 29% or 2.61.
References #
- Hawker GA, Mian S, et al. Measures of adult pain. Arthritis Care Res 2011; 63 (Suppl 11):S240-52.
- www.rehabmeasures.org
- Downie WW, Leatham PA et al. Studies with pain rating scales. Annals Rheum Dis 1978; 37(4):378-81.
- Gagliese L, Weizblit N, et al. The measurement of postoperative pain: a comparison of intensity scales in younger and older surgical patients. Pain 2005; 117(3):412-20.
- Finch E, Stratford PW, Mayo NE. Physical Rehabilitation Outcome Measures. 2nd ed:Canadian Physiotherapy Association; 2002.
- Spadoni GF, Stratford PW, et al. The evaluation of change in pain intensity: a comparison of the P4 and single-item numeric pain rating scales. J Orthop Sport Phys Ther 2004; 34(4):187-93.
- Farrar JT, Young JP Jr, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001; 94(2):149-58.
- Sloman R, Wruble AW, et al. Determination of clinically meaningful levels of pain reduction in patients experiencing acute postoperative pain. Pain Management Nurs 2006; 7(4):153-8.
- WHO International Classification of Functioning, Disability, and Health – http://www.who.int/classifications/icf/icf_more/en/
- Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. F.A. Davis Company: Philadelphia.
