Description #
This course will address some of the non-pharmacological approaches for managing pain and the importance of biopsychosocial interdisciplinary team approaches as well as roles.
Learning Objectives #
At the end of this course the health care professional will be able to:
- a.Describe & understand the concept of total pain management
- b.Understand the importance of the biopsychosocial interdisciplinary team approach to pain management
- c.Describe key interdisciplinary team member roles in helping with the non-pharmacological management of pain
- d. List and understand at least 5 non-pharmacological approaches for pain management
- e. Experience at least one non-pharmacologial approach or coping skill for pain management
Introduction:
Most pain management treatments have revolved around the medicinal drugs which have been only beneficial to the treating the physical aspect of Pain. Medicinal drugs have been only effective to a certain limit. The purpose of this module is to provide information relating to Non-Pharmacological Approaches to Pain Management. It gives an in-depth explanation on the multi-disciplinary approach to pain management through non-pharmacological methods. This module includes an overview, explanation on the concept of pain, many examples of non-pharmacological pain treatments, description of specific roles of each interdisciplinary members and Pain flash presentation (at the end of module). The goal of non-pharmacological pain treatment is to minimize pain, improve function and increase the quality of life.
Overview #
A brief overview of Non-Pharmacological Approaches of Pain Management:
Management of pain through a variety of non-pharmacological intervention helps make pain:
- More tolerable
- Decrease analgesic requirements
- Improve functional ability
- Decrease emotional component of pain
- Enhance coping strategies
Non-pharmacological approach is a non-drug measure for management that may be used alone or in conjunction with pharmacological therapy to optimize pain management. It is also known as Complementary and Alternative Medicine (CAM). It is non-drug measurement for pain management and there is a growing scientific evidence regarding the efficacy of non-drug measures (Ernest, Pittler and Wider, 2007). Total Pain management requires a multimodal interdisciplinary approach using both non-pharmacological and pharmacological approaches. Upto 73% of Canadians have used CAM therapies at least once in their life (Esmail, 2007; McCaffery and Pasero, 1999).
Examples of non-pharmacological interventions:
- Acupuncture
- Transcutaneous Electrical Nerve Stimulation
- Spinal Cord Stimulator
- Massage
- Exercise/Physical Therapy
- Hot or cold application
- Therapeutic touch/Reflexology
- Meditiation
- Education/Counseling
- Cognitive Behavioural Therapy
- Hypnosis
- Distraction/Visual Imagery
The cycle of pain:
This cycle is common with both acute and chronic pain. Increased pain, causes increases anxiety which results in increased muscle tension. Non-pharmacological approaches to pain help break the cycle of pain by decreasing anxiety and muscle tension thereby decreasing the person’s pain.
The Pain-Relieving Anti-nociceptive System:
The body’s pan relieving or anti-nociceptive system balances out the pain-sensing system.
Certain type of stimuli can trigger activation of anti-nociceptive system. These stimuli are:
- Exercise
- Meditation
- Being Comforted
- Reassured as in patient education/counselling
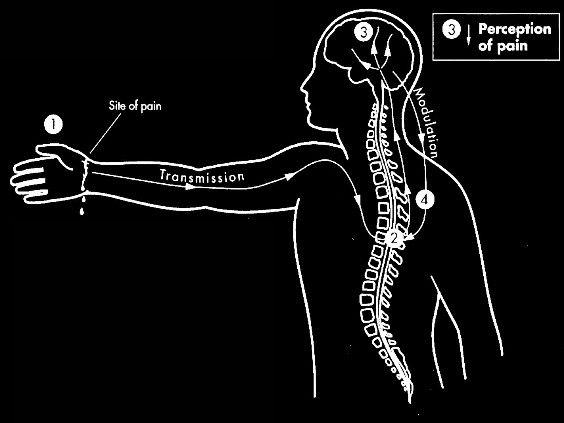
This explains the utility of many of the behavioural components of pain management programs. The perception of pain is modified as the brain can only process so many supratentorial inputs and if it is focusing on meditation, hypnosis, relaxation, music, etc. It will be unable to process the pain signals so the message of the pain can be decreased. This occurs in addition to the pain relieving anti-nociceptive system which works in most people when pain signals transmitted by peripheral nerves or nociceptor, arrive in the brain, they activate neurons in the periaqueductal gray matter of the brain and the nucleus raph magnus of the brainstem, which release endorphins and enkephalins.
Endorpins bind to mu-opioid receptors on pain sensing nerves in the periphery and spinal cord, inhibiting the propagation of more pain signals. Enkephalins bind to delta opioid receptors in the spinal cord, causing spinal neurons to release gamma-aminobutyric acid (GABA), alpha-2-adrenergic mediators, oxytocin, relaxin and other chemicals that dampen the pain signals in the spinal cord. Also, serotonin and norepinephrine are sent down to the dorsal horn of the spinal cord. Most medication used for pain relief mimic the actions of these natural analgesic agents.
This pathway is shown in the diagram below.
Perception of Pain:
With the use of non-pharmacological approaches, the increased supratenorial inputs into the brain decrease the perception of pain, as the brain can only process so many inputs at one time.
The diagram below explains the perception of pain:
Understanding the concept of total pain #
Concept of Total Pain:
Previous pain management modules have described Pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or describe in terms of such damage.”
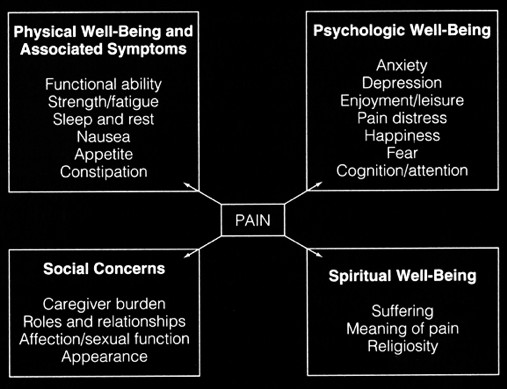
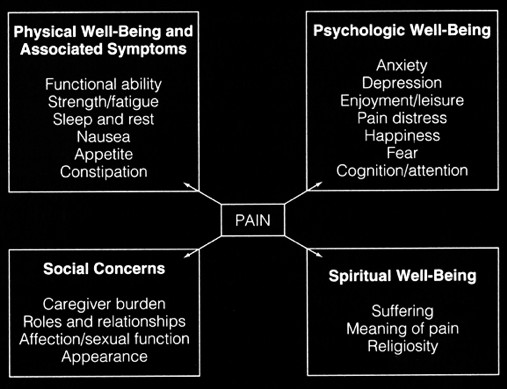
Studies have shown that uncontrolled pain negatively affects the immune system, promotes cancerous growths and can compromise health leading to increased mortality rate. Pain consists of four main components: Physical, Psychological, Social and Spiritual Aspects. The figure below shows the four different aspects of pain. One of the main hurdle in pain management is that most health professionals are only trained to treat the physical aspects of pain. Often, it is very difficult to identify the social and spiritual components of pain. Nowadays, an interdisciplinary approach is taken to deal with all four aspects of pain. An interdisciplinary team can address the physical component, family distress, social isolation and spiritual loss.
This figure explains the four different aspects of Pain and provides some example for them.
Importance of biopsychosocial interdisciplinary team approach #
Pain is an invisible common problem and its management is one of the most complex issues in medicine today. Pain affects not only physically but it has a major impact on the social, psychological, social and spiritual aspects of a person’s life. Since pain is a multidimensional experience, its management can be taking by an interdisciplinary approach. Combined efforts of many health care professionals as interdisciplinary team are needed to effectively manage the multitude of factors contributing to patient’s perception of pain. Interdisciplinary method have shown greater long-term improvement than a single modality method or omission of treatment.
Interdisciplinary pain team members includes:
- Patient and family.
- Nurses
- Physicians
- Pharmacist
- Psychologist
- Social Worker
- Occupational therapist/ Physiotherapist
- Pastoral care
Key Roles of Interdisciplinary team members #
It takes combined efforts of many health care professional as an interdisciplinary team to provide effective management if the multiple factors that contribute to the person’s perception of pain. Only by understanding the functions of each discipline represented on a team can one truly understand how each discipline contributes to achieving the team goals.
The following key disciplines are briefly reviewed:
Patient and Family:
In effective pain management it is crucial to involve the patient and family as equal partners in the development of a treatment plan. they should be involved in determining which members of the interdisciplinary team to include in the management of pain and in the formulation of treatment goals.
Nurse:
The role of the nurse is often considered central to the pain management team and is often the team’s formal leader. In many instances RN’s who lead the team in additional training and certification in nursing specialties such as diabetes, hospice, oncology or pediatrics.
Nursing activities on the pain management team are quite broad and can include: the comprehensive assessment of the patient, ensuring direct patient involvement in the management of pain, documentation of current medications-including drug allergies and sensitivities; obtaining a comprehensive medical history; administration and teaching about medications; reassessing response to treatment; monitoring the patient for side effects or complications of treatment; collaborating wit the physicians on the pain management team regarding the patient’s response to treatments and obtaining any necessary changes in therapy; and collaborating with other members of the pain team. such as social workers, chaplains and pharmacists in providing comprehensive pain management to the patient.
Physician:
A variety of physician specialists may participate as members of the pain management team such as anaethesiologists, neurosurgeons, psychiatrists, pharmacologist-internists, rheumatologists, medical oncologists and family physicians.
This large number of different types of medical specialists are consulted due to the multi-factorial nature of pain-needing approaches such as nerve blocks, spinal cord stimulator insertion and emotional/psychological factors needing to be addressed for good pain management to occur.
Pharmacist:
The role of the pharmacist has become appreciated as integral to an effective pain team. In addition to dispensing medication, pharmacists collect, organize and evaluate information; formulate a plan; provide medications, education and counseling; and monitor and manage patient outcomes.
Pyschologist:
The professional skills of the psychologist are needed to manage complex psychosocial aspects of a patient’s pain.
Social Worker:
The social worker has two functions first as a liaison between the patient-family and the social community network. Second as a counselor, the social worker provides a source of support to the patient and family as they consider treatment options, changes the family roles and opening communication within the family and between providers of care.
Occupational Therapist:
An occupational therapist works to restore self-care and work-related skills in the patient who experiences performance deficits.
Physiotherapist:
A physical therapist examines and treats individuals with physical limitations to correct or alleviate those disabilities usually with exercises or ultrasound/heat treatments, etc.
Pastoral Care/Champlain:
Many patients, especially those suffering from cancer pain, wonder if their pain is something they must endure as a form of divine punishment for something they did in this life. The chaplain on the pain management team may be the best professional to address this concern assuring the patient that pain relief is the proper goal. The chaplain can also answer other spiritual questions as well.
Miler, B.; Bruno, S. & Kinzbrunner, B. team approach to pain management, In Salerno, E. & Wilkens, J.S. (1997). Pain Management handbook: An interdisciplinary approach. Toronto, ON: CV Mosby Inc., 179-200.
Non-pharmacological Interventions for pain management #
Non-Pharmacological Interventions:
- Hot or Cold Therapy
- Exercise/Physical Therapy
- Transcutaneous Electrical Nerve Stimulation (TENS)
- Relaxation
- Cognitive Behaviour Therapy
- Soothing Touch
- Music Therapy
- Visual (Guided) Imagery/Distraction
- Meditation
- Hypnosis
- Patient/Family Education
Hot or Cold Therapy
“Mechanism of Action”: Decreases sensitivity to Pain.
This type of therapy is beneficial for muscle pain, muscle spasm and visceral pain. Cold therapy is a very effective therapy immediately post injury and for the first 48 hours to 72 hours. It reduces blood circulation at the injured resulting in reduced swelling. Heat therapy increases circulation at the injured site resulting in increased swelling and pain. Heat therapy should never be used immediately post injury. Alternating heat/cold therapy for 15 minutes every 4 to 6 hours produces best results. If cold therapy relieves pain, it can be more effective than heat. Also, it is an easily understood concept by patients and their families.
Cold Therapy is also known as cryotherapy. It can be applied via ice packs, towels soaked in iced water or chemical gel packs. It relieves pain associate with sprains and strains prior to applying heat. It is effective for acute rheumatoid arthritis pain, episiotomy pain and headache as well. This type of therapy be used cautiously in patients who have a history of frostbite, hypertension and in areas of nerve injuries.
In addition, Cold should not be used:
- With patients who are cold insensitive or have an aversion to cold. In rare cases, people are cold insensitive and have a reaction that is similar to an allergic reaction.
- With patients who have a medical condition that effects circulation including: Raynaud’s Disease, systemic lups erythematous (SLE), peripheral vascular disease (PVD) or scleroderma.
Hot Therapy is also known as thermotherapy. The effects of heat do not last as long as cold, but can give a temporary relief for up to an hour or more. It can be applied via hot packs, hot water bottles, hot and moist compresses, electric heating pads, topical analgesic rubs/lotions, chemical gel packs or immersion in hot water. The temperature should be warm not hot to prevent the risk of burns. Immersion in warm water should be done cautiously in those who experience orthostatic hypotension. It can be effective during the subacute and chronic stages on an injury. It is very beneficial in relieving neck or low back pain, joint pain and rectal pain.
A topical analgesic rubs/lotion and heat should not be used at the same time as it increases the risk of burns. Patients should wait 1-2 hours after applying an analgesic rub before using heat. Heat should not be used:
- In the acute stage of an injury.
- By patients who have decreased or impaired sesation such as: with diabetic neurophathy, stroke, head injury and nerve damage.
- Where there is compromised circulation such as: Peripheral Vascular Disease (PVD), arterial insufficiency, cardiac conditions and diabetes.
- Over malignant tumors, over open wounds or areas of suspected infection or an area with moderate to severe edema.
Mayo Foundation, 2006, McCaffery and Pasero, 1999.
Physical Exercise
“Mechanism of Action”: It is effective in:
- Strengthening muscles
- Improving coordination
- Balance
- Mobility
- Function
- Mood and Comfort
Many evidence shows that physical exercise benefits a wide range of acute and chronic musculoskeletal conditions including low back pain and fibromyalgia. It is an activity that is usually enjoyable, comfortable to do and benefits are easily recognized. Successful participation in an exercise program reduces fear of re-injury.
Jovey, Boulage, Clark et al. 2008.
Transcutaneous Electrical Nerve Stimulation (TENS):
“Mechanism of Action”: Low voltage electrical current used in stimulating body’s endogenous opioids and block nociceptive activity in the spinal cord used to treat pain.
It is thought to work by stimulating the body’s endogenous opioids and block the nociceptive activity in the spinal cord. Research evidence regarding the effectiveness of TENS is mixed. TENS may be useful adjunct in the management of mild to moderate cancer pain, osteoarthritis, neuropathic pain and angina. This procedure is contraindicated in patients with epilepsy, cardiac pacemaker and in pregnancy as it may induce early labor.


Patients are instructed to try different frequencies and intensities to find those that provide the best pain control for that individual. Optimal settings of stimulus parameters are subjective and are determined by trial and error. Electrode positioning is important; it must be placed initially on the skin over or contralateral to the painful area but other locations such as over cutaneous nerves, trigger points, acupuncture sites may give similar or even better pain relief.
Kaye, V (2005). Transcutaneous Electrical Nerve Stimulation. E-medicine.
Http://www.emedicine.com/pmr/topic206.htm#section~introduction
Relaxation:
“Mechanism of Action”: Reduces muscle tension and anxiety thereby reduces pain.
Some of the relaxation techniques include slow deep rhythmic breathing and progressive/active relaxation. It can also include visual imagery. Evidence exists that relating reduces chronic pain in a variety of medical conditions.
This video elaborates a relaxation technique that includes visual imagery and soothing music/voice.
Cognitive Behavioural Therapy:
“Mechanism of Action”:
- Modification of patient’s thoughts feeling and beliefs regarding their pain.
- Modification of learned behavioural responses to pain.
It does not eliminate pain but changes a patient’s perception of pain from overwhelming to manageable. CBT is commonly used for persistent (chronic) pain. Studies have shown that CBT can improve the patient’s sense of control over chronic pain and improve function. This therapy changes the patients’ perception of their pain from ‘overwhelming’ to ‘manageable’.
This therapy teaches:
- Coping skills so patients can better manage their pain and associated issues.
- How to regain some control over their life by managing suffering.
- Skills such as distraction, relaxation, pacing that they can apply to their daily life.
- To anticipate problems and plan solutions within their abilities.
- The association between thoughts, feelings and behaviours and to identify and change maladaptive pain related behaviours.
Jovey R, Boulanger A, Clark A, 2008; McCaffery and Passero, 1999.
Soothing Touch:
“Mechanism of Action”: Decreases anxiety and tension.
It includes:
- Acupuncture/Acupressure
- Massage therapy
- Healing touch/Therapeutic Touch
- Tension releasing exercises
Ernest, Pittler and Wider, 2007; Rakel, 2008.
Acupuncture is a traditional Chinese non-medicinal procedure of penetrating skin with thin, solid, metallic needles that involves stimulation of anatomical points on the body. Also, it is thought to stimulate the body’s endogenous opioids.
It has been effective relieving dental pain, chronic back pain and migraines. Adverse effect are rare but include infection (trough non-sterile needles) and tissue trauma. In some provinces, acupuncturist are regulated.
Ho, 2001; MacPherson, Thorpe, Thomas and Campbell, 2003.
Massage Therapy is an application of touch or force to soft tissues without movement of joints. It promotes muscle relaxation and decreases anxiety or tension. A growing body of research shows massage therapy can be an effective part of pan relief and management. Massage therapists are regulated health professionals.
Massage therapy provides relief from:
- Headaches
- Persistent low back pain
- Muscle pain and spasms

Tsao, 2007; Ernst, 2009.
Healing touch/Therapeutic touch is an energy therapy that uses touch to influence the human energy system and the energy field surrounding the body. This type of therapy restores harmony and balance in the energy system. It is a non invasive technique which leads to physical, emotional, mental and spiritual healing. Recent scientific research have shown that healing touch promotes relaxation, reduce pain and manage stress.
Tension releasing Exercises…………
Music Therapy:
“Mechanism of Action”:
- The body responding physiologically to sounds and vibrations of music.
- Changing neronal activity with entrainment to musicla rhythms in lateral termporal lobe and cortical areas of brain devoted to movement.
Music is an intentional auditory stimulus with organized elements including melody, rhythm, harmony, timbre, form and style.
Rawal et al (2005) study showed:
- Introperative music may decrease post-operative pain.
- Post operative music therapy may reduce anxiety, pain and morphine consumption.
Kemper, Dnahauer 2005; Rawal et. al 2005.
Visual (Guided) Imagery is a relaxation technique that guides the mind into a calm and still state. It involves the mind imagining positive images in order to bring healthy and positive change. Guided imagery can be achieved via audiotape, soothing music, sounds of nature and/or pictures. It is a simple yet powerful tool in pain management.
Example: Visual Imagery can be obtained by using a photo album of trip.
Distraction
“Mechanism of Action”: Distraction is based on a person’s limited capacity to allocate attention to more than one ask at a time.
It involves directing attention away from pain. The potential benefits of distraction are increased pan tolerance and decreased pain intensity. Distraction places attention on a stimulus other than pain places pain in the periphery of awareness. Potential adverse effects of distraction after the distraction is over include an increased awareness of pain, fatigue, doubt of the existance of pain.
Two different coping techniques utilize distraction.
These techniques are:
- Mindfulness meditation
- Hypnosis.
Waters SJ, Cognitive Behavioral Pain Management. In:Dworkin, RH, Breitbat SW, editors.
Psychosocial Aspects of Pain: A Handbook for health care providers. Series: Progress in pain research and management, vol 27. Seattle, WA: IASP Press, 2003, p273-4.
Mindfulness meditation is a conscious discipline involving the cultivation of non-judgmental, moment-to-moment awareness in one’s life. This procedure focuses on breathing and yoga techniques to help strengthen muscles.
Kabat-Zinn, 1996.
Hypnosis is a broad concept and has been used for numerous purposes. Therapy with hypnosis (hypnotherapy) involves the use of many techniques, one of which is imagery. All hypnosis is self-hypnosis) sometimes directed by another person) and that hypnotic thinking is a state of alertness and intense concentration, very similar to normal everyday thinking.
Ernest, Pittler and Wider, 2007.
Patient/Family Education:
“Mechanism of Action”: Educating patients and their families about pain and management of pain has shown to decrease anxiety, pain intensity and disbeliefs regarding pain management.
The Canadian Pain Society position statement identifies that the “best pain management involves patients, families and health professionals”. The society focuses on the providing information on pain management. Education provides a forum to give patients info regarding communicating their pain to the health care team and address any questions or concerns. It can be provided in verbal, written, audio/video/CD ROM formats.
Some of the benefits are:
- Identification and clarification of misbelief
- Correct medication self-administration, prevention of side effects
- Increased control over pain
- Less fear of addiction, decreased pain
References:
- Belgrade M. & Huntoon E.(2009). A Primer on Acupuncture. Clinical Health Affairs, 40-43
- Brookoff D.(2000) Chronic Pain. 1. A New Disease. Hospital Practice, 35(7)45-52,59
- Esmail,N.(2007) Complementary and alternative medicine in Canada: trends in use and public attitudes, 1997-2006, Fraser Institute.
- Ernst, E.; Pittler,M.H.;& Wider, B.(2007). Complementary therapies for “pain management”an evidence based approach. Philadelphia, PA:Elsevier Mosby
- Ernst E. (2009).Supportive Care in Cancer. Spring Berlin/Heilelberg 9, 17(4): 333-337
- Frey LA, Evans S, Knudtson J, Nus S, Scholl K, Sluka KA.(2008) Massage Reduces Pain Perception and Hyperalgesia in Experimental Muscle Pain: A Randomized, Controlled Trial. The Journal of Pain, 9(8): 714-721
- Jovey R, Boulanger A,& Clark A et. al.(2008) Managing Pain The Canadian Healthcare Professional’s Reference. Baker Edwards Consulting Inc.
- Kaye, V. (2005). Transcutaneous Electrical Nerve Stimulation. E-medicine http://www.emedicine.com/pmr/topic206.htm#section~introduction
- Kemper KJ, Danhauser SC.(2005). Music as Therapy. Southern Medical Journal, 98(3): 282-288
- MaCaffery M,& Pasero C.(1999) Pain: Clinical Manual, 2nd ed. St. Louis, MO: Mosby, Inc.; p 742
- Mannerkorpi K. (2007)Non-pharmacological treatment of chronic widespread musculoskeletal pain. Best Practice & Research Clinical Rheumatology, 21(3): 513-534
- Oliver DP, Wittenberg-Lyles E, Demeris G, Washington K, Porock D, & Day M. (2008).Barriers to Pain Management: Caregiver Perceptions and Pain Talk by Hospice Interdisciplinary Teams. Journal of Pain Symptom Management, 36(4): 374-382
- Pesco MS, Chosa E, &Tajima N. (2006). Comparative Study of Hands-On Therapy With Active Exercises vs Education With Active Exercises for the Management for Upper Back Pain. Journal of Manipulative and Physiological Therapeutics, 29(3): 228-235
- Park J, Linde K,& Manheimer E. (2008). The status and future of acupuncture clinical research: Journal of Alternative Complementary Medicine, Sept. 14(7): 871-881
- Rakel D. Healing or Therapeutic Touch and Reiki Therapy: Integrative Medicine 2nd Edition. Philadelphia, PA: Saunders Elsevier, Inc.
- Tam LS, Leung PC, Li TK, Zhang L,& Li EK. (2007). Acupuncture in the treatment of rheumatoid arthritis: a double-blind controlled pilot study. BioMed Central Complementary and Alternative Medicine, 7:35
- Tsao J.(2007). Effectiveness of Massage Therapy for Chronic Non-Malignant Pain
- Verhoef MJ, Vanderheyden LC, Dryden T, Mallory D, Ware MA.(2006). Evaluating complementary and alternative medicine interventions: in search of appropriate patient-centered outcome measures. BioMed Central Complementary and Alternative Medicine, 6:38
- Waters SJ.(2003) Cognitive behavioral pain management. In: Dworkin RH, Breitbat SW, editors. Psychosocial Aspects of pain: A handbook for health care providers Series: Progress in pain research and management, volume 27.Seattle, WA: IASP Press, p 273-4.
- Weingarten T.(2006) Mayo Foundation Medical Education and Research. Expert Guide to Pain Management, 2006
