Description #
This unit is aimed at providing information on the potential complications that could occur during the administration of Procedural Sedation and Analgesia and the appropriate treatments/management.
Learning Objectives #
At the end of the session the student will be able to :
- a) Be familiar with the potential complications related to PSA and the interventions required to effectively manage these complications
- b) Identify and master the use of the essential necessary equipment to handle the emergency situation
ANTICIPATION AND MANAGEMENT OF COMPLICATIONS
For Procedural Sedation and Analgesia, complications can arise from any combination of:
- The drug therapies administered
- The procedure itself
- The patient’s underlying comorbidities
For the nurse monitoring the patient, (s)he must be astutely aware of:
- Patient’s baseline vital signs
- Physical assessment findings
- Subtle signs of problems or complications
This unit will focus on some common problems associated with Procedural Sedation:
- Risk factors
- Causes
- Recognition
- Interdisciplinary management
- Risk factors for respiratory management problems
- A history of:
- Problems with anesthesia or sedation e.g.: malignant hyperthermia
- Abnormal craniofacial anatomy
- Morbid obesity
- Neck abnormalities such as limited movement, short neck or advanced arthritis (rheumatoid arthritis)
- Sleep apnea, snoring, stridor
UPPER AIRWAY
- Nasopharynx: lies behind the nasal cavity, extends from the level of the junction of the hard and soft palates to the base of skull
- Oropharynx: from soft palate to the hyoid bone {a u-shaped bone between the mandible and the larynx}
- Laryngopharynx: from the hyoid bone, diverging posteriorly to connect with the esophagus and anteriorly into larynx)
- The opening to the larynx is covered by the epiglottis
- Epiglottis is a large, leaf-like structure that moves freely to prevent aspiration of gastric contents from the oropharynx into the trachea
- To avoid gastric acid aspiration, it is advisable that the gag reflex be maintained during the administration of PSA medications
- The trachea extends from the larynx to the 5th thoracic vertebrae
- The trachea lies anterior to the esophagus and bifurcates into the right and left main-stem bronchi
- The right and left bronchi progressively branch to eventually form the terminal bronchioles
LOWER AIRWAY
ORAL / NASAL AIRWAY SIZING CHART
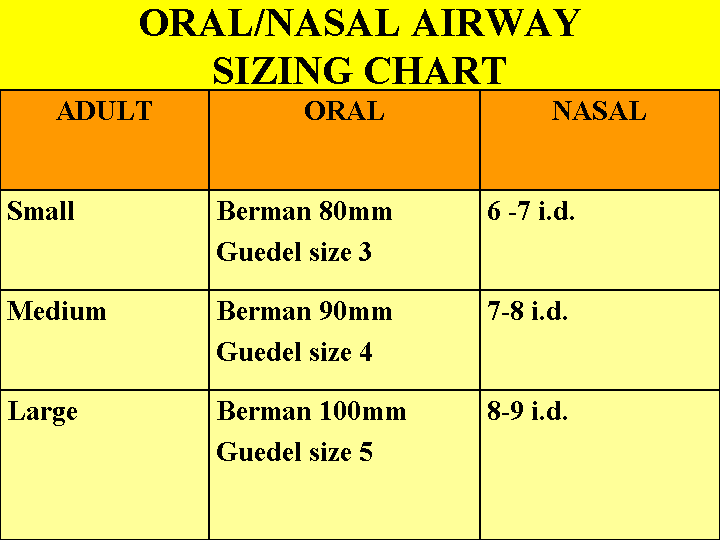
NASAL AIRWAY SIZING
NASAL AIRWAY INSERTION
ORAL AIRWAY SIZING
ORAL AIRWAY INSERTION
ASSESSMENT
- Patient assessment is consistent with the ABC’s of resuscitation –
- A Airway
- B Breathing
- C Circulation
- The ability to positionally maintain an open airway should be assessed and documented through physical examination (Malampati Technique) and by determining the level of consciousness and arousability of the patient
- Observation of the patient before, during and after the period of sedation is crucial
- Discrete changes in patient status are often observed before noticeable changes in vital signs and other parameters occur
- Baseline level of consciousness prior to the sedation should also be assessed and documented
- Breathing should be assessed through the use of continuous pulse oximetry and observation of respiratory rate, depth and effort during PSA; ETCO2 monitoring during deep sedation
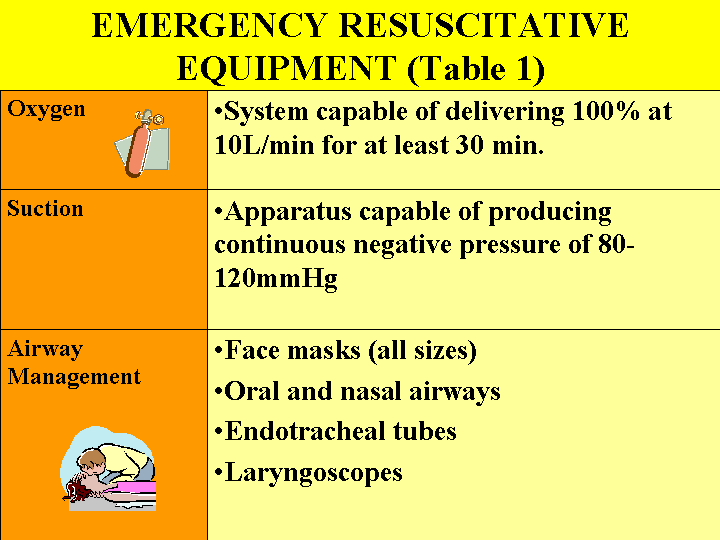
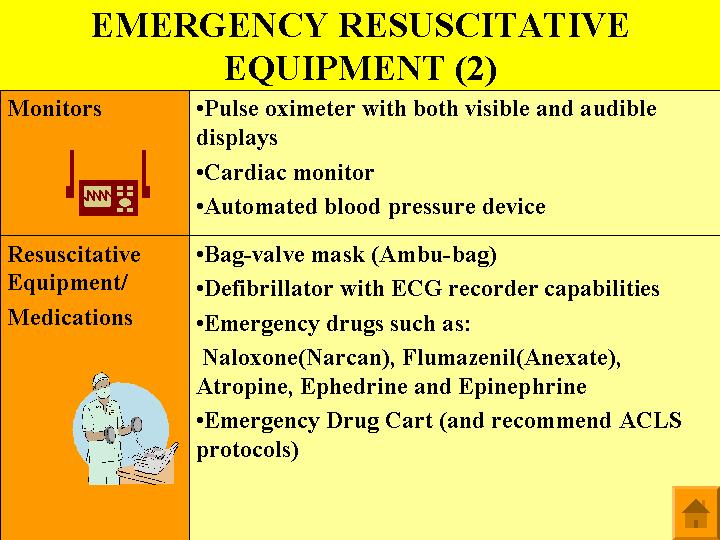
EQUIPMENT AND SUPPLIES
- The physician and nurse’s responsibility must focus on assessing parameters that may be impacted by PSA medications
- Prior to sedating the patient, the health care practitioner needs to ensure that all monitoring equipment required for PSA (see TABLE 1&2) is present and functioning
Most Common Complications -Upper Airway Obstruction #
UPPER AIRWAY OBSTRUCTION
- Takes on various forms
- Mechanical airway obstruction occurs when patients inadvertently move into deeper levels of sedation and are unable to maintain their own airway
- Repositioning the patient may cause airway obstruction; therefore, it mandates an immediate reassessment of airway patency
TREATMENT FOR AIRWAY OBSTRUCTION
- For adults:
- Performing a jaw thrust may be necessary to open the patient’s airway
- If the patient is unconscious, an oral or nasal airway should be inserted
•Artificial airways are used to maintain the patency of the patient’s airway: oral, nasal, laryngeal mask and ETT
•Oral and nasal airways hold the tongue away from the posterior wall of the pharynx allowing the unconscious patient to maintain an unobstructed airway
To size for an oral airway:
•Measure distance from the corner of the patient’s mouth to the earlobe
•The airway is inserted with the point towards the roof of the mouth and then rotated into position at the back of the throat
To size for a nasal airway (a soft rubber or plastic tube):
•Measure from the tip of the nose to the earlobe
•Apply lubricant (water-base jelly) and insert gently into one nostril
•If resistance is encountered; a slight rotation will facilitate insertion. If persistently resistant, then try the other naris
CHIN LIFT
JAW THRUST
BAGGING
BURP
- The ‘BURP’ maneuver (consisting of backward, upward and right-sided pressure on the thyroid and cricoid cartilages) is the technique used to facilitate direct visualization of a slightly anterior larynx
- The maneuver is performed by placing the thumb and middle finger on the cricoid cartilage and the index finger is placed on the left hand side of the lower portion of the cricoid cartilage
CRICOID PRESSURE
- Cricoid pressure (Sellick maneuver) is used to temporarily occlude the upper end of the esophagus
- The maneuver is most often used to help align the airway structures during endotracheal intubation and to provide a means of preventing gastric insufflation and vomiting during ventilations in an unprotected airway
- The cricoid cartilage is the only upper airway cartilaginous structure that is a complete ring
- The esophagus begins at the lower portion of the cricoid cartilage; thus pressure anteriorly will compress the esophagus against the anterior vertebral body of the sixth cervical vertebra (C6)
- Too little = increased risk of aspiration
- Too much = airway obstruction
- Rapid sequence with Sellick’s maneuver (Full stomach and Cricoid pressure)
- Pre-oxygenation
- Rapid injection of hypnotic (without titration)
- Rapid injection of muscle relaxant (immediately afterwards)
- Cricoid pressure at loss of consciousness
- No ventilation until intubation confirmed
- Source : http://www.medstudents.com.br/anest/anest2f1.html
ENDOTRACHEAL TUBE
Supplies required to assist intubation by the Anesthesiologist:
An assortment of Endotracheal tube sizes (#6,6.5,7,8,9) must be kept on hand at all times

- Stylet-provides rigidity to the tube
- Laryngoscope handle and blade –used to manipulate the oropharyngeal tissue and epiglottis. Selection of a blade depends on patient age, and anatomical variabilities as well as clinician preference

- Magill forceps- used to direct the OETT
- Suction equipment- liners, tubing and catheters
LARYNGEAL MASK
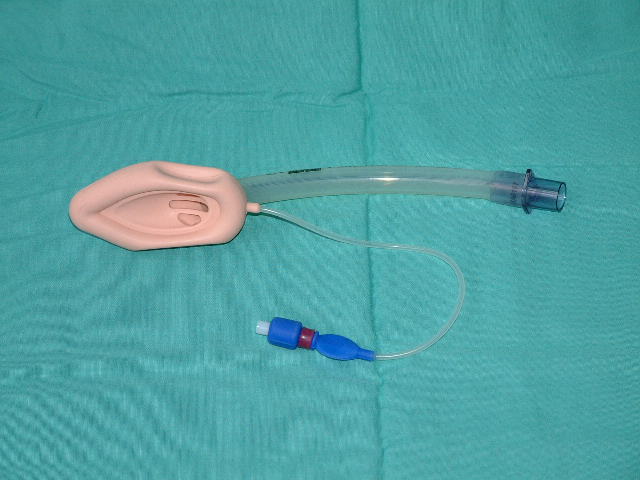
- The LMA is inserted blindly by the Anesthesiologist into the pharynx and forms a low pressure seal around the laryngeal inlet
- It is easily placed and a clear, unobstructed airway may be obtained in virtually all patients
- The LMA is not an alternative to the endo-tracheal tube but rather, it should be considered an alternative to the face mask when it is not possible to effectively ventilate and oxygenate a patient through a face mask or after failed attempts to intubate
- The airway is occasionally completely or partially obstructed after placement of the LMA and this is usually related to down- folding of the epiglottis or in-folding of the aryepiglotic folds
- However, unlike an endotracheal tube, a laryngeal mask cannot protect the airway or lungs from aspiration of regurgitated material, and deep (subglottic) suctioning cannot be performed through the mask
AIRWAY COMPLICATIONS ASSOCIATED WITH USE OF ARTIFICAL AIRWAYS
Complications can arise from:
- Mouth, nose or throat trauma related to forceful insertion
- Airway obstruction – the artificial airway is malpositioned or too long, and occludes the epiglottis or rests in the esophagus
- Precipitation of vomiting and laryngospasm in semi-conscious and conscious patients
- Then pressure is applied to both of these structures downwards, superiorly and to the
- right hand side (patient’s)
LARYNGOSPASM
- A form of airway obstruction (spasm of the vocal cords) requiring immediate recognition and emergent care
- It can cause partial or complete airway obstruction
Precursors to this airway problem include:
- Age (1-4yrs)
- History of asthma, smoking and/or COPD
- Accumulated secretions in the back of the throat (sputum, saliva or blood)
- Procedures involving the neck, throat, sinuses or nose
- Semi-conscious and conscious patients with oral or nasal airways
- Obesity
- Sleep apnea
- Short neck
- Parkinson’s disease
- “Light” sedation
- Hypoxia
- Allergic reactions
- Frequent suctioning or coughing
Signs and Symptoms:
**Can be mild, but are usually dramatic. If the patient is awake, they will be extremely frightened
- Hoarse voice
- Stridor
- Barking or brassy cough
- Supraclavicular indrawing
- Nasal flaring
- Rocking chest
- Rapid drop in oxygen saturation
Emergency Management:
- Focus on maintaining a patent airway
- Promote ease of breathing
- Reduce patient anxiety
- Treat the vocal cord spasm
- Inform the physician
- Allay anxiety – THIS IS CRITICAL!!
- Apply a jaw thrust
- Position the patient to promote ease of breathing
- Provide cool humidified oxygen (often at 100%)
- Monitor the respiratory rate, breath sounds, overall air entry and other vital signs including oxygen saturation
- Administer nebulized medications to open the “tense vocal cords”-Racemic epinephrine 2.25% (0.5ml diluted in 3ml preservative free N/S)
Effects last about 2 hours – monitor closely for a reoccurrence once the drug has worn off,
***Bronchodilators –Ventolin/Atrovent have little or no benefit.
RESPIRATORY DEPRESSION
- Respiratory depression and lower airway obstruction can lead to various levels of hypoxia and hypercapnea.
- Patients with respiratory insufficiency may have a variety of S& S such as :
- a) Hypoventilation
- b) Dyspnea
- c) Wheezing
- d) Tachycardia
- e) Anxiousness
- f) Low oxygen saturation
- g) Elevated ETCO2
- Risk factors:
- Obesity
- Pregnancy (3rd trimester)
- Impaired gag/cough reflex
- Respiratory muscle weakness
Comorbidities and high ASA level
- Smoking
- Advanced age
- Chest/abdominal procedures
- Emergency procedure
- Upper airway obstruction
- Pain
- Long term procedure (>1hr)
- Pre-medications (sedatives/narcotics)
Treatment:
- Is demonstrated by decreased or shallow respirations and decreased oxygen saturation
- Maintain the ABC’s (airway, breathing, circulation)
- Should be treated with oxygen, airway management and administration of reversal agents as needed
- If the condition does not improve, call for assistance/call a code and prepare for intubation
RESPIRATORY DEPRESSION CAN PROGRESS TO RESPIRATORY ARREST!!!
- If the patient is breathing and has adequate oxygen saturation but cannot maintain their airway, an artificial airway is indicated
- A nasal or oral airway may be used
- In the conscious patient, a nasal airway may be better tolerated
INTRA-PROCEDURAL ASPIRATION
Can be caused by:
- A full stomach
- Gastric distention
- Intestinal spasm causing reflux of stomach contents
- Passive aspiration during the procedure
- Aggressive hyperventilation with face/laryngeal mask
- Nature of procedure
Due to the tracheal anatomy, with the
downward slope of the right main bronchus,
aspiration of gastric contents usually occurs in the right lung field
Clinical Manifestations:
- Cough
- Tachypnea
- Sputum production
- Tachycardia
- Low oxygen saturation
- Dyspnea
- Wheezing
- Crackles over right lung field
- Pleural rub
- Throat suctioning returns that look like stomach contents
Treatment:
- Nebulized bronchodilators
- IV antibiotics
BRONCHOSPASM
Can be due to:
- An upper airway obstruction
- Asthma
- Allergic reaction side effect
- Exposure to allergens (i.e. Latex
Signs & Symptoms include:
- Dyspnea
- Wheezing
- Pursed lip breathing and or nasal flaring
- Wide-eyed facial expression
- Difficulty speaking more than a few words
- Prolonged expiration
- Chest tightness
- Low oxygen saturation
Treatment includes:
- Nebulized bronchodilators
- Epinephrine (sc) and IV steroids
- Magnesium sulphate (IV)
- Aminophylline
SEVERE ASTHMA
- Can lead to death
- Catecholamine excess and associated hypoxia contribute to this fatal event
Cardiac arrest in asthma patients is associated with:
- Cessation of wheezing which may indicate worsening distress
- Severe bronchospasm leading to asphyxia
- Cardiac dysrhythmias
- Use of adrenergic agonists
- BP & HR mediated by vasovagal reflexes
NEGATIVE PRESSURE PULMONARY EDEMA
Possible causes:
- Upper airway obstruction – laryngeal edema and/or spasm
Signs &Symptoms:
- Usually becomes apparent when the airway obstruction is relieved
- Sudden decrease in oxygen saturation
- Uni or bilateral crackles
- Dyspnea/tachypnea
- Pink frothy sputum
MANAGEMENT OF RESPIRATORY INSUFFICIENCY
Overall goals include:
- Maintaining a patent airway (including intubation)
- Promoting adequate gas exchange
- Restoring acid-base balance
- Identifying and treating the underlying cause(s)
Initial interventions for emergency management are:
- Apply oxygen to maintain O2 sat>95%
- Monitor respirations (rate & character), airway, breath sounds
- Have emergency airway equipment on standby (ambu-bag, airways, intubation equipment)
- Ensure IV access
- Assess for central or peripheral cyanosis
Initial interventions for emergency management are:
- Position to promote ease of breathing (use of accessory muscles, in-drawing, nasal flaring, inability to speak)
- Monitor LOC
- Monitor ECG rhythm, HR & BP
- Obtain blood work (ABG, Lytes)
- Prepare for tests (12 lead ECG, CXR)
Assist with/initiate drugs and therapies specific to the underlying cause:
- Drug induced-administer reversal agents
- Bronchospasm- nebulized bronchodilators, Racemic Epinephrine, administer Epinephrine (sc), and IV steroids, Magnesium sulfate and Aminophylline
- Negative pressure pulmonary edema-once a cardiac cause has been ruled out, positive pressure ventilation (BiPAP) or intubation with mechanical ventilation, IV Morphine and Nitropatch
- IV Morphine and Nitropatch to reduce venous return, IV Midazolam for anxiety, IV diuretics (Lasix) to remobilize the fluid.
HYPOTENSION
- A drop of 20-30% below normal pressure that issustained for more than a few minutes
Possible causes:
- Pre-existing health issue
- Response to medication and hypovolemia
- Vaso-vagal response
Treatment includes:
- Assess for likely causes (i.e.bleeding,
- hypovolemia, bradycardia)
- Administer or increase oxygen
- Administer fluids
- Administer drugs related to the cause
- Continue to assess BP/HR every 1-5 minutes
- Make sure airway is patent
- Monitor pulse oximetry
- Stimulation of the vagus nerve
- May be caused by anxiety of procedure and is usually self limiting
- Symptoms are diaphoresis, bradycardia, hypotension and loss of consciousness
- Removal of stimulus and arousal of patient is usually all that is necessary
- Have Atropine available
- Position change if permitted (i.e.Trendelenberg)
HYPERTENSION
Possible causes:
- Pre-existing hypertension
- Increased level of circulating catecholamines
- Antihypertensive drugs not taken
- Pain
- Bladder distension
- Shivering
- Rigidity associated with Fentanyl and neuroleptic/antiemetic drugs (e.g. Droperidol)
- Volume overload
- Hypoxia
- Hypothermia with vasoconstriction
Treatment includes:
- Monitor BP/HR, pulse oximetry, respiratory rate and pattern, air entry and oxygen therapy
- Analgesics
- Sedation
- Assess intake and output
- Antihypertensives (beta blockers, ACE inhibitors)
- Check for bladder distention and catheterize PRN
PAIN
- Is the most common experience with patients undergoing invasive procedures
- Important to determine if cause is related to procedure or complication
- In patients with altered states of consciousness, pain may be expressed through physiologic signs such as changes in heart rate, blood pressure, respiratory rate and delirium
- Frequent assessments for pain are essential (type, location, onset, intensity, duration, triggers and relief)
Common causes:
- Operative site
- Procedural positioning
- Bladder distention
- Procedural complication
- Pre-existing health problems
Methods to control pain include:
- Pre and post procedure use of nonsteroidal anti-inflammatory drugs (NSAIDS)
- IV opioid
- Diversional activities (music)
- Topical application or cutaneous infiltration of a local anesthetic
- Regional anesthesia/analgesia
If unrelieved, pain can contribute to many complications:
- Hypo/hyperventilation
- Agitation
- Tachycardia
- Hypertension
CARDIAC DYSRHYTHMIAS
- Any underlying cardiac rhythm problems should be corrected particularly if causing symptoms
- Cardiac dysrhythmias are a serious complication of Procedural Sedation and must be recognized and treated quickly
- Tachycardia- most serious are PVC’s and Atrial dysrhythmias (which may be caused by hypoxemia)
- Bradycardia- most common
Potential causes:
- Underlying cardiac disease
- Myocardial infarction and ischemia
- Effects of analgesia
- Vagal effects
- Hypoventilation
- Anxiety
- Fluid imbalance
- Hypotension/hypertension
- Hypovolemia / hypervolemia
- Electrolyte and acid-base imbalances
- Hypothermia
Common treatments include:
- Ongoing assessment of: HR, BP, O2Sat
- Treat underlying cause
- Administer or increase oxygen
- Administer fluids
- Administer anti-arrhythmia drugs
AGITATION / DELIRIUM
Manifestations include: combativeness, severe restlessness, disorientation and persistent moaning, crying and screaming
- Important to identify and treat the underlying cause
Possible causes include:
- Hypoxia
- Airway obstruction
- Pain
- Full bladder
- Fluid, electrolyte and acid-base imbalances
- Adverse effects of medications
- Drug interactions
- Withdrawal from alcohol or other drugs
- Ketamine-hallucinations or unpleasant dreams
- Inconsistent reactions to drugs
- Pre-existing mental states (i.e.dementia, depression)
Treatment includes:
- Identify the underlying cause
- Initiating specific therapy
- Protecting the patient from injury
NAUSEA & VOMITING
- A common consequence of Procedural Sedation
Conditions and circumstances contributing to nausea and vomiting include:
- Age/gender (ェrisk in children & elderly)
- Obesity
- Pre-procedure anxiety
- History of nausea and vomiting
- Predisposition to motion sickness
- Gastric distention
- Full stomach prior to the procedure
- Drug effects
- Pain
- Hypotension
Treatment:
- Refer to the Antiemetic Drug information supplied in the Drug Pharmacology Unit
BLEEDING
- Procedures associated with Procedural Sedation have a lower incidence of major hemorrhage
- Assessments for bleeding focus on observing for both obvious and occult signs
Some obvious signs:
- Frank oozing at the procedural site-always look under the patient as fluid / blood will follow gravity and flow downward
- Excessive losses through drainage systems
- Swelling or hematoma formation at the site. The abdomen can hold over a litre of fluid/blood before any signs of distention are seen
- There are no absolute symptoms that diagnose shock, and not all patients with shock present in a similar manner
- Many of the traditional symptoms associated with shock are the outcome of the body’s compensatory mechanisms which focus on preserving vital organs (e.g. Stimulation of the antidiuretic hormone mechanism and the renin-angiotensin-aldosterone mechanism)
- The diagnosis of shock should not be limited to one or two textbook signs like hypotension or tachycardia
- In compensated hypovolemic shock, a patient’s heart rate may be less than 100, with a BP slightly higher than normal
- Elderly or beta-blocked patients may not produce a compensatory tachycardia in response to excessive blood loss
Some classic signs:
- Flat neck veins with clear lung fields
- Unexplained tachycardia
- Hypotension
- Dramatic drop in BP following administration of IV Morphine
- Tachypnea
- Restlessness, anxiousness, irritability
- Unrelieved pain at or near the procedural site
- Decreased urine output
- Vasoconstriction- poor capillary refill- gray, pale skin
ALLERGIC RESPONSE
- Anaphylaxis is a life threatening reaction involving IgE immunoglobulin
- Assess if localized or systemic
* It is helpful to ascertain the cause of the allergic response
Symptoms include:
- Bronchospasm
- Hives
- Confusion
- Facial edema
- Wheezing
- Urticaria
- Oropharyngeal edema
- Cardiac compromise
- Hypotension due to histamine release
Treatment for allergic reaction will depend on the symptoms and cause:
- Remove or discontinue suspected allergen
- Airway maintenance
- Increase intravenous volume
- Prepare Epinephrine if cardiac compromise
- Have Diphenhydramine, Bronchodilators, Corticosteroids and Aminophylline readily available
COMMON COMPLICATIONS CHARTS
Cyber Patient Module

PATIENT PROFILE:
Name: Anne Urick,
Anne Urick is a 57-year-old female with a remote history of IV drug use from which she developed hepatitis C, she had a liver transplant in 1994, which has been complicated by multiple biliary obstructions requiring stenting and reconstruction post-transplant. The latest was 2 weeks ago she has had mild to moderate abdominal pain since and was placed on Cipro when she went to follow-up in the clinic. She presented today in the ER with weakness, fever and increasing abdominal pain. Since she arrived she has had labs drawn, a chest x-ray, ECG, abdominal ultrasound and a contrast abdominal CT scan. No results are back yet but she is stable.
Current Orders:
- Dx post op infection
- VSR
- NPO
- I + 0
- IV D51 / 2NS with 20mEq KCI @125/hr
- Meds
- Cyclosporine 85mg PO BID
- Immuran 100mg PO BID
- Ciprofloxicin 500mg PO BID
- Tylenol 325mg PO Q6h pm for Temp > 38.5°C
- Tylenol #3 ii PO Q6h PRN for abdominal pain
- Tylenol #3 ii PO Q6h PRN for abdominal pain
- Blood cultures X 2 for Temp > 38.5
Video #
Procedural Sedation video for procedures longer than 20 minutes.
Procedural Sedation video for procedures shorter than 20 minutes.
OBJECTIVE REVIEW
1) Describe the potential complications related to PSA and the interventions required to effectively manage
these complications
2) Identify and describe the essential necessary equipment to handle emergency situations
REFERENCES
BC Cancer Agency. (2002) Conscious Sedation Learning Module.
Kost, M., (2004). Moderate Sedation: Core competencies for practice, 2nd edition. Permission obtained for 14 pages only including 2 Figures and 5 Tables
Kost, M., (1998). Manual of conscious sedation, W.B. Saunders CO. Saunders Elsevier, St. Louis, MO
Lions Gate Hospital (2001). Conscious Sedation & Nursing Implications Educational module
MacFarlane (2000) BCIT. Peri-Procedural Nursing care of patients receiving conscious sedation and analgesia, 1-74
Practice guidelines for sedation and analgesia by non-anesthesiologists. An updated report by the American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. (2001). American Association of Anesthesiology.
Robins, E., Bozadjian, E., (1997). Developing a Competency Based Program for Conscious Sedation.
Snider, D., Clarke, D., Finucane, B, (2005). The “BURP” maneuver worsens the glottic view when applied in combination with cricoid pressure. Canadian Journal of Anesthesia -Cardiothoracic Anesthesia, respiration and Airway; 52: pp 101
Vancouver Community College Continuing Education (2002). Conscious Sedation (HLTH 1182) Nursing Management: Pre-procedural to Post-operative Teaching. 1-59. Material used from Pages 4,18 &19 with permission.
