Description #
This unit will describe the correct administration, scoring and interpretation of the KOOS for TKA patients.
Learning Objectives #
By the end of this unit, the learner will be able to perform the following tasks for Total Knee Arthoplasty patients:
– Administer the KOOS
– Score the KOOS
– Interpret the KOOS
What is this test? #
What is the KOOS? #
The Knee injury and Osteoarthritis Outcome Score (KOOS) is a valid, reliable, and responsive measure for assessing TKA patients and falls within the WHO’s ICF domains of Body Function or Structure and Activity (Figure 1). The KOOS assesses pain; other symptoms such as swelling, restricted ROM and mechanical symptoms; function in daily living (ADLs); function in sport and recreation (Sport/Rec); and knee related quality of life (QoL) over the past week. Since it is a comprehensive test, it will take ~15-20 minutes for it to be completed and scored.
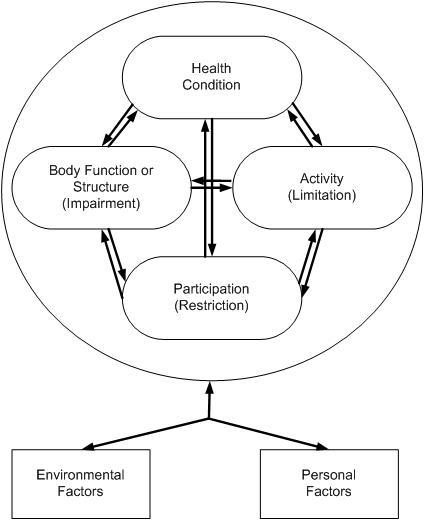
Figure 1. The International Classification of Functioning, Disability and Health (ICF) Conceptual Model. Taken from Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. Figure 2-1.
When do I use it? #
When do I use the KOOS? #
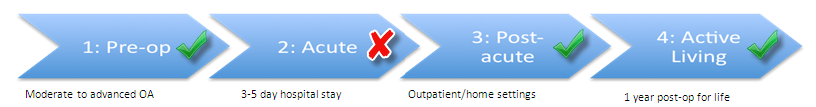
The Knee injury and Osteoarthritis Outcome Score (KOOS) can be used in a number of phases along the TJA Continuum of Care. Specifically, as seen in Figure 2, the KOOS is recommended for use in the Pre-Operative, Post-Acute, and Active Living phases of the TJA continuum. Health professionals can therefore use this outcome measure to monitor change in the patient’s status as he or she moves through these phases of the care (*note that it is not recommended in the Acute phase).
Figure 2. The phases along the TJA Continuum of Care for which the KOOS is recommended.
Equipment needed? #
What equipment is used to complete the KOOS? #
The equipment that is required will depend on how you have the patient complete the KOOS. If internet access is not available, either at your clinic or the patient’s home, the patient will require:
- A paper copy of the KOOS which can be found here → Link to the Paper Version of the KOOS
- A pen
If your clinic or the patient has internet access, then an electronic version of the KOOS is available for the patient to complete at the link below.
Please bookmark the link on your web browser so you can access the KOOS quickly whenever you need it.
While the KOOS is lengthy (as it requires the patient to respond to 42 questions), its value lies in its ability to capture many aspects of the patient’s experience (i.e. symptoms/stiffness, pain, function, sport, and quality of life).
How do I do it? #
How do I administer the KOOS? #
Since this is a patient reported outcome measure there is very little that you need to do. Just ensure that the patient has access to the paper or online version of the KOOS and have them follow the instructions at the top of the page. When they are finished it will then need to be scored.
- Are you interested in learning more about the KOOS? If so, visit the official KOOS website to learn more!
- Do you want all the module information on a single piece of paper? If so, click this link → KOOS One Pager
How do I score it? #
How do I score the KOOS? #
Scoring the Knee injury and Osteoarthritis Outcome Score (KOOS) is easy to do:
- If the patient has completed the paper version of the KOOS a spreadsheet for scoring is available at www.koos.nu.
- If the patient has completed the electronic version of the KOOS, then it will be automatically scored for you.
- Just in case you have not bookmarked the electronic version of the HOOS in your internet browser yet, the link to it can be found below.
Link to the Electronic Version of the KOOS
Data Tips! #
What do I do when items have been incorrectly marked or left blank on the KOOS? #
In some instances, your patient may have incorrectly marked or left items blank on the KOOS. Not to worry! The authors of the KOOS have compiled some examples of patient errors and how best to address them.
If the patient1:
- places a mark outside the check box. → Choose the box closest to the mark.
- marks two boxes instead of one. → Choose the box that indicates the more severe problem.
- answered < 50% of the subscale items in an individual subscale. → Then the individual subscale is considered invalid and no score should be calculated from that subscale.
- answered > 50% of the subscale items in an individual subscale → Then the subscale is considered valid.
To calculate the subscale score when > 50% of the items in an individual subscale are answered, you must calculate the mean score (average) within the subscale. If you are using the Excel spreadsheet provided at the KOOS homepage, then this will be automatically calculated for you. If you are using a paper copy of the KOOS, then take a look at the Example subheading under Data Tips! for guidance.
The minimum number of items completed for each subscale are as follows:
- 5 or more items from the Pain subscale must be answered
- 4 or more items from the Symptoms subscale must be answered
- 9 or more items from the ADL subscale must be answered
- 3 or more items from the Sport/Rec subscale must be answered
- 2 or more items from the QoL subscale must be answered
Example #
Example #
Mr. S has had a left TKA 3 weeks ago and has come to you for rehab. You choose the KOOS as your PROM and give it to Mr. S to complete. Mr S returns the KOOS and when reviewing the Pain subscale (Figure 3) you see the following:
Figure 3. The Mr. S’s Pain subscale of the KOOS. Modified from www.koos.nu
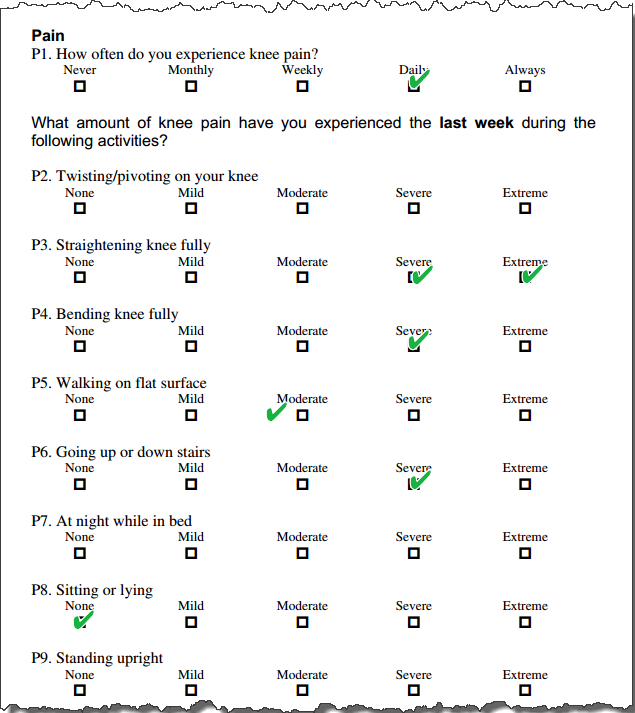
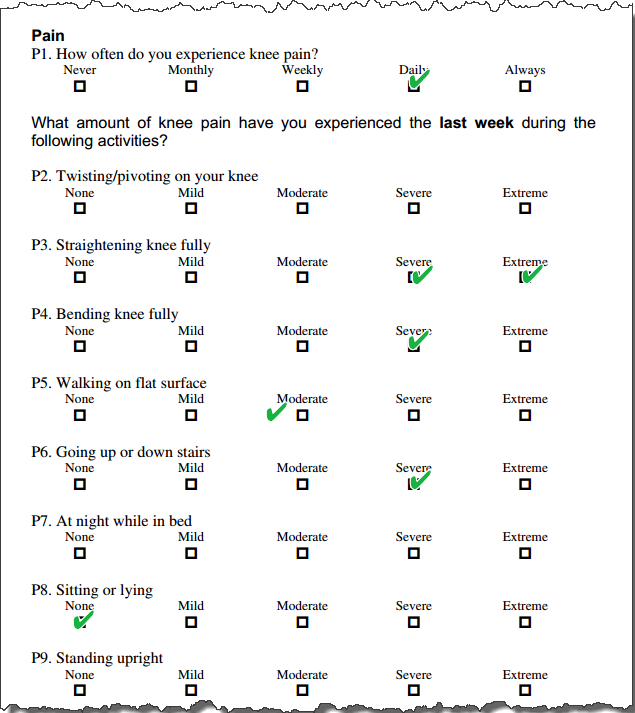
Figure 4. KOOS Scoring Instructions.
Taken from Knee injury and Osteoarthritis Outcome Score (HOOS) Scoring Instructions
Please answer the following questions:
- What is the correct answer for P3.?
- What is the correct answer for P5.?
- What is the score for the Pain subscale of the HOOS?
Answers:
1. What is the correct answer for P3.?
Answer: Extreme. If two boxes are marked, the box which indicates the more severe problem is chosen.
2. What is the correct answer for P5.?
Answer: Moderate. If a mark is placed outside a box, the closest box is chosen.
3. What is the score for the Pain subsection?
Answer: 38.
How did I get it?
1. Determine the values for each of items in the Pain subscale using Figure 4.
P1. = 3
P2. = no answer
P3. = 4
P4. = 3
P5. = 2
P6. = 3
P7. = no answer
P8. = 0
P9. = no answer
2. Use the following equation:
Subscale Score = 100 – {[(x)/y]/4}*100,
Where
- x = the total of the completed item values added together
- y = the number of completed item responses in the subscale
= 100 – {[(x)/y]/4}*100
= 100 – {[(3+4+3+2+3+0)/6]/4}*100
= 100 – {[15/6]/4}*100
= 100 – {2.5/4}*100
= 100 – 0.625*100
= 100 – 58.3
= 37.5
= 38 (rounded)
#
What does it mean? #
How do I interpret the KOOS? #
It is simple to interpret the Knee injury and Osteoarthritis Outcome Score (KOOS) – the higher the score, the better. For example, a score of 100 in each subscale indicates no knee-related problems while a score of 0 indicates extreme knee problems. In addition, changes in the subscales can assist you in identifying if your treatment has caused TRUE CHANGE in the patient. For example, in patients with knee OA the following MDC values were found for each of the subscales:
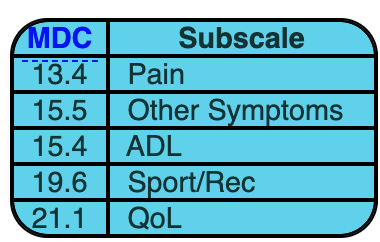
What does this mean for my patient? It means that in patients with knee OA, the change in score between test occasions must be greater than MDC value for the subscale in question, in order to reflect a true change and not just measurement error.
To get a better understanding of how to use the MDC in practice, please go to the examples section.
- While MDC values have been calculated for each of the subscale categories in the KOOS, the MDC has not been calculated for total score.
Examples #
Mr. S is a patient with knee OA who is receiving treatment from you while awaiting TKA. You have used the KOOS as your PROM and found the following information listed in the Table 1:
Table 1
 #
#
Using the information in the Table 1 and Table 2, please determine if true change occurred in each of the KOOS subscales?
Table 2
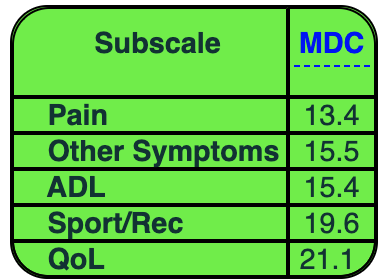
Has true change occurred in the Pain subscale? #
1. Calculate the change in score between test occasions
45.23 – 22.22 = 23.01
2. Compare the MDC to the change in score
23.01 > 13.4
Yes, true change did occur because the difference in score between test occasions is greater than the MDC of 13.4 for the Pain subscale.
Has true change occurred in the Other Symptoms subscale? #
1. Calculate the change in score between test occasions
57.01 – 42.86 = 14.15
2. Compare the MDC to the change in score
14.15 < 15.5
No, true change did not occur because the difference in score between test occasions is less than the MDC of 15.5 for the Other Symptoms subscale
Has true change occurred in the ADLs subscale? #
1. Calculate the change in score between test occasions
38.52 – 19.12 = 19.4
2. Compare the MDC to the change in score
19.4 > 15.4
Yes, true change did occur because the difference in score between test occasions is greater than the MDC of 15.4 for the ADLs subscale.
Has true change occurred in the Sport/Rec subscale? #
1. Calculate the change in score between test occasions
20.01 – 10.00 = 10.01
2. Compare the MDC to the change in score
10.01 < 19.6
No, true change did not occur because the difference in score between test occasions is less than the MDC of 19.6 for the Sport/Rec subscale
Has true change occurred in the QoL subscale? #
1. Calculate the change in score between test occasions
49.18 – 25.00 = 24.18
2. Compare the MDC to the change in score
24.18 > 21.1
Yes, true change did occur because the difference in score between test occasions is greater than the MDC of 21.1 for the QoL subscale.
References #
- Website with users guide: www.koos.nu/
- Roos E, Engelhart L, et al. ICRS Recommendation Document: Patient-reported outcome instruments for use in patients with articular cartilage defects. Osteoarthritis Cartilage. 2011;2(2):122-36.
- Roos EM, Roos HP, et al. Knee Injury and Osteoarthritis Outcome Score (KOOS) – development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88-96.
- Rehabilitation Measures Database. www.rehabmeasures.org/Lists/RehabMeasures/PrintView.aspx?ID=1011
- Collins NJ, Misra D, et al. Measures of physical performance assessments. Patient Outcomes in Rheumatology: A Review of Measures. Arthritis Care Res. 2011;63(11):S208.
- Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS) – validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003;1:17.
- Roos EM, Lohmander LS. Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64.
- WHO International Classification of Functioning, Disability, and Health – http://www.who.int/classifications/icf/icf_more/en/
- Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. F.A. Davis Company: Philadelphia.
