Surgical instruments have prehistoric roots in Indian, Chinese, Babylonian, Egyptian, and Roman civilizations. Today, hundreds of surgical instruments are used for specific functions or are designed to serve a common task.
The aim of this content is to introduce basic surgical instruments that are used for common surgical procedures.
- Scalpel
- Scissors
- Sutures
- Needles
- Needle Holders
- Forceps
- Retractors
Scalpel
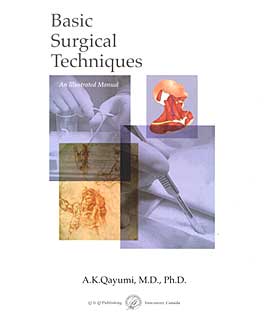
A scalpel is used for the division of tissue and consists of a blade and handle. Although some scalpels are made of one solid piece of steel that includes both the handle and blade, the majority of scalpels have a separate handle and a removable blade. Blades are available in a variety of shapes, each designed for a specific purpose. The most common blades have a straight back and an oval-shaped sharp cutting front.

The most commonly used blade sizes are #10, #20, and #22 (Figure 1.2). Figure 1.3 demonstrates other designs of scalpel blades which include a bayonet tip blade #11(a), a bistoury blade #12(b), and a small blade #15(c). Handle #4 fits into larger blades (#’s 20, 21, 22, 25) (Figure 1.2) and handles #3, 7, and 9 fit into smaller blades (#’s 10, 11, 12, 15) (Figure 1.3).

Scissors
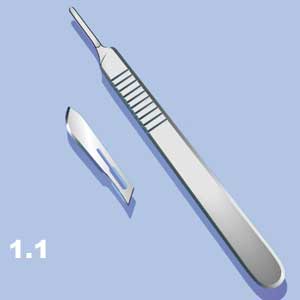
Scissors are used for cutting, dissecting, and debriding tissue. They may also be used for cutting sutures, bandages, and dressings. Scissors can either be long or short and/or with blades that are straight or curved. Their tips can be both sharp, one sharp and one blunt, or both blunt. Mayo and Metzenbaum scissors are two basic types of scissors for tissue dissection. Metzenbaum scissors (or “Mets”) are the favorite among surgeons as they are lighter and longer instruments with a gentle curve near the end.
Scissors are used for cutting, dissecting, and debriding tissue. They may also be used for cutting sutures, bandages, and dressings. Scissors can either be long or short and/or with blades that are straight or curved. Their tips can be both sharp, one sharp and one blunt, or both blunt (Figure 1.4). Mayo (Figure 1.5) and Metzenbaum (Figure 1.6) scissors are two basic types of scissors for tissue dissection. Metzenbaum scissors (or “Mets”) are the favorite among surgeons as they are lighter and longer instruments with a gentle curve near the end. Figure 1.7 demonstrates bandage scissors.



NB: Mayo scissors are used for heavy, hard, and thick tissue as well as sutures, gauze, tubes, etc. Metzenbaum scissors, on the other hand, are used for tissue dissection and fine work only. Do not cut sutures or other materials with Mets.
Sutures
A suture is a strand of material used to ligate (tie) blood vessels or approximate (sew) tissues. The use of plant strings or animal sinews for wound closure was described by many ancient civilizations (e.g. Chinese, Babylonians, Greeks). In the past, many materials have been used for this purpose: dried gut, dried tendon, strips of hiding, horsehair, human hair, bark fibers, etc. The word “suture” is commonly used to refer to a suture with a needle for sewing, whereas a suture without a needle, used for tying, is referred to as a “tie”. The tie may either be “free”, referring to a straight strand of suture material or on a “reel”, where the suture is on a spool for multiple ligatures.
Suture materials can be classified by:
a) structure – monofilament and multifilament
b) behavior in tissue – absorbable and non-absorbable
c) origin – organic, synthetic, or metallic
Structure
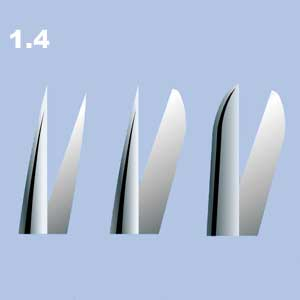
i. Monofilament sutures (Figure 1.8) are made of a single strand of material and therefore encounter less resistance than multifilament sutures when passing through tissue. They also resist harboring organisms that may cause suture tie infection. Monofilament sutures must be handled with care as crushing or crimping of the suture can nick or create a weak spot in the strand which may result in suture breakage.
ii. Multifilament sutures (Figure 1.9) consist of several filaments rendered into a strand by spinning, twisting or braiding. This provides greater tensile strength and pliability, but multifilament sutures can harbour infectious organisms between strands.

Behaviour in Tissue
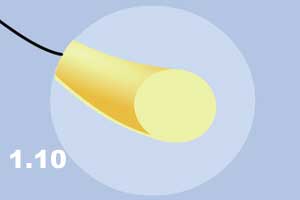
Absorbable sutures are made from the collagen of healthy mammals (e.g. catgut) or from synthetic polymers (e.g. polyglycolic acid). They are used for temporary tissue approximation until sufficient wound healing has occurred to withstand normal stress. One major difference between the materials is that knots from synthetic material are more likely to slip than knots tied with biologic suture material. Organic (natural) absorbable sutures are absorbed into tissue after digestion by proteolytic enzymes, whereas synthetic absorbable sutures are hydrolyzed when water gradually penetrates the suture filaments and breaks down the polymer. Absorbable sutures may be organic (e.g. catgut) or synthetic (e.g. polyglycolic acid). Catgut (Figure 1.10) is made from the submucosa of sheep intestine or the serosa of bovine intestine and is 98% collagen. Plain catgut maintains tensile strength for only 7-10 days and is completely absorbed within 70 days.
Origin
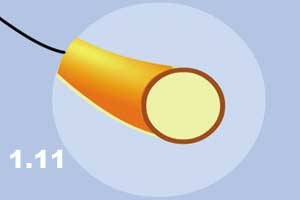
In the second half of the 19th century, Lister treated catgut with chrome in order to prolong its life in vivo. The life of chromic catgut is about 3 months (90 days).
The chromizing process alters the coloration of the surgical gut from yellowish-tan to brown (Figure 1.11).
Chromic gut sutures maintain tensile strength for 10-14 days and cause less tissue irritation than plain gut.
Synthetic absorbable materials are primarily made of polyglycolic acid and its modifications (Figure 1.12).
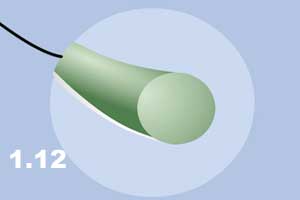
The most widely used synthetic absorbable materials are POLYSORB®, DEXON®, PDS®, VICRYL®, BIOSYN®, and MAXON®. These materials are primarily monofilaments and are absorbed into the tissue in about 90 days. Approximately 65% of original tensile strength is maintained at 14 days. Hydrolyzation of synthetic polymers causes less tissue reaction than enzymatic digestion of chrome. This is an important consideration in the surgeon’s suture choice.
The most frequently used non-absorbable materials in surgery are silk, linen, cotton, and synthetic materials such as polyester (DACRON® O), polyamide (nylon), polyolefins (SURGIDAC®, SURGILENE®, PROLENE®), and polyester (NOVAFIL®, SURGIPRO®).
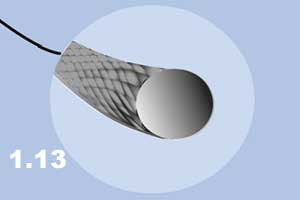
Silk is commonly used by surgeons (Figure 1.13) as it handles well and holds knots (i.e. does not slip). It is classified as nonabsorbable, however, in vivo studies have shown that it loses tensile strength in about one year and cannot usually be detected in tissue after 2 years. Therefore, in reality, silk is a very slow absorbing suture and hence should not be used in situations where long-term support of tissue is required.
Metallic sutures, such as stainless steel and silver wire (Figure 1.14) are both commonly used in surgery today. Metallic sutures are indicated in areas of known infection and/or when it is desirable to avoid excessive tissue reaction. Other uses of metallic wire are in orthopedic and plastic surgery repair of bones, ligaments, and cartilage.
The diameter of sutures can vary from 0.013 mm to 1.016 mm. The size of the suture is directly related to the diameter of the thread. Size 0 is about .5 mm thick. When the diameter of the thread is smaller than 0.5, a “0” is added to the number, when it is larger, only the number is displayed for the size of the suture. For example, “2-0” is thinner than “1-0” and “7-0” is thinner than “6-0” but size “2” is thicker than size “1”.
Needles
The surgical needle is as important as the suture. A surgical needle can be divided into three parts: the point, the body, and the tail or suture attachment end. The point is the sharp end of a needle, which can have a variety of shapes and configurations. The most widely used needle points are called “taper” and “cutting”. The taper needlepoint is round and is designed for soft tissue such as bowels or blood vessels. The body of the needle and the thread follow the tapered point and seal the hole made by the needle. This prevents bleeding or evacuation of microbes through the walls of contaminated cavities such as bowels.
The cutting needlepoint has at least two, and often three, opposing cutting edges. These sharp edges enable the needle to go through tough tissue, such as skin, by cutting it. The cutting needle is used for hard tissue such as skin or fascia where the cutting of tissue does not create a danger for infection, bleeding, or other complications.
The body of the needle may have different shapes. It can 1/2, 3/8, 5/8, 1/4 of a circle, or straight. The tail of the needle has either an eye for the suture to be loaded or is swaged (atraumatic or “eyeless”)
Chart #
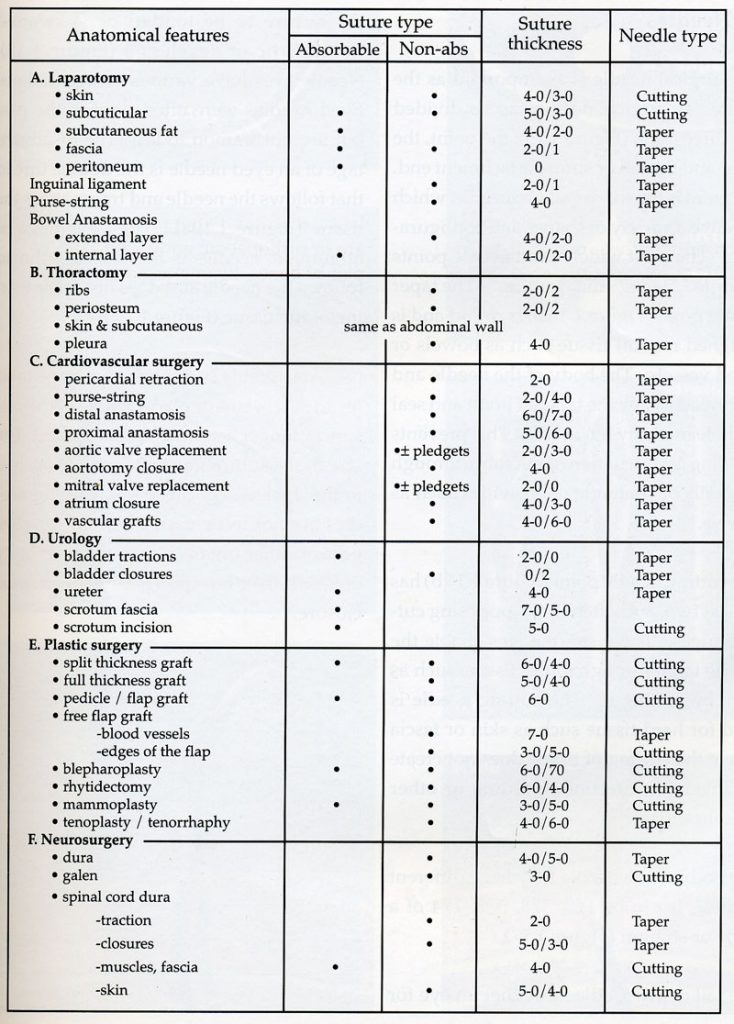
Needles #
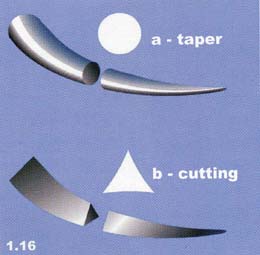
The surgical needle is as important as the suture. A surgical needle can be divided into three parts (Figure 1.15): the point, the body, and the tail or suture attachment end. The point is the sharp end of a needle, which can have a variety of shapes and configurations. The most widely used needle points are called “taper” and “cutting”. The taper needlepoint (Figure 1.16a) is round and is designed for soft tissue such as bowels or blood vessels. The body of the needle and the thread follow the tapered point and seal the hole made by the needle. This prevents bleeding or evacuation of microbes through the walls of contaminated cavities such as bowels.
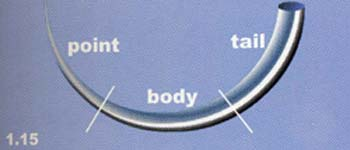
The cutting needle point (Figure 1.16b) has at least two, and often three, opposing cutting edges. These sharp edges enable the needle to go through tough tissue, such as skin, by cutting it. The cutting needle is used for hard tissue such as skin or fascia where the cutting of tissue does not create a danger for infection, bleeding or other complications
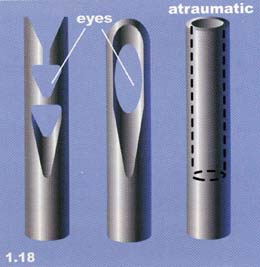
The body of the needle may have different shapes. It can 1/2, 3/8, 5/8, 1/4 of a circle or straight (Figure 1.17). The tail of the needle has either an eye for the suture to be loaded or is swaged (atraumatic or “eyeless”) (Figure 1.18).
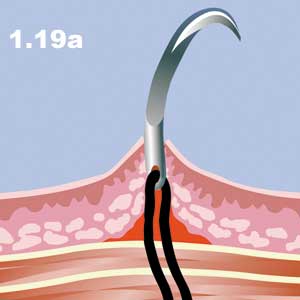
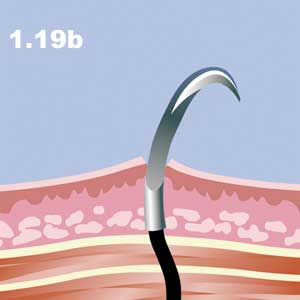
Needle eyes have various configurations. Eyed needles were often used in the past but are uncommon today. The disadvantage of an eyed needle is the double thread that follows the needle and traumatizes the tissue (Figure 1.19a). The advantage of atraumatic needles is that a single thread follows the needle and does not cause tearing of the tissue (Figure 1.19b).
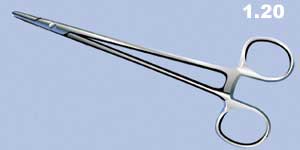
Needle Holder
A needle holder (driver) is a surgical instrument that provides a firm grasp for a needle to be manipulated at a distance from the suture target. Needle holders have a variety of jaws and handles. The most commonly used needle holder has rings on the end of the handle (like scissors), a short blade jaw to hold the needle, and usually a locking mechanism (ratchet) (Figure 1.20).
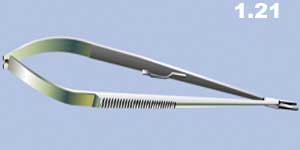
The second type, or Castroviejo needle holder (Figure 1.21), does not have rings but instead consists of two strips of metal joined at one end with locking devices between them.
The jaws of a needle holder have a variety of configurations designed to provide a firm grip on different sized needles (Figure 1.22).

Forceps
The word “forceps” describes different types of surgical instruments:
a) thumb grasp
b) grasping forceps
c) hemostatic forceps
d) other types of forceps
a) Thumb forceps consist of two strips of metal joined at one end and are used to pick up tissue or hold tissue between opposed surfaces, thereby giving a surgeon more control over the amount of pressure applied to the tissue. The needle “tips” or “heads” on the opposing surfaces of forceps create a variety of designs specific to the use of the instrument.

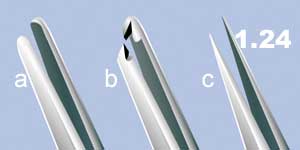
i) if the tips are blunt, the instrument is called a dressing forceps (Figure 1.24a).
ii) if the branches have teeth, or are serrated, it is called tissue forceps (Figure 1.24b).
iii) if the branches are sharp, it is called splinter forceps (Figure 1.24c).
b) Grasping forceps are designed to hold tissues strong enough to allow one to exert traction. The opposing heads vary depending on the instrument’s specific purpose. All have a set of finger grips and a locking mechanism.
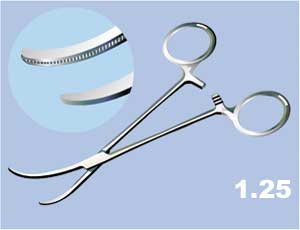
i) Debaky forceps are a special type of forceps that have a flat endpoint covered with fine teeth and a longitudinal groove (Figure 1.25).
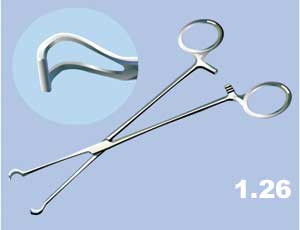
ii) Figure 1.26 demonstrates a Babcock clamp (forceps) used for grasping delicate tissue and tubular structures, e.g. vermiform appendix or fallopian tube. This instrument has curved empty triangular branches and the base of each triangular opposes one another.
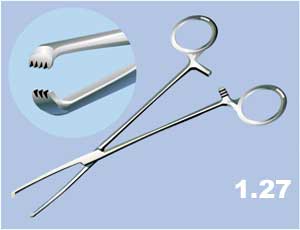
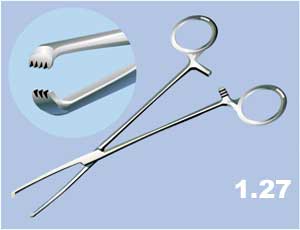
iii) The Allis clamp (forceps) has opposing serrated tips with short teeth used for grasping touch tissues such as fascia (Figure 1.27).
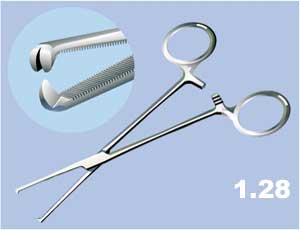
iv) A Kocher clamp (forceps) has short transverse serrations along the length of the blades and the tips have sharp teeth (Figure 1.28).
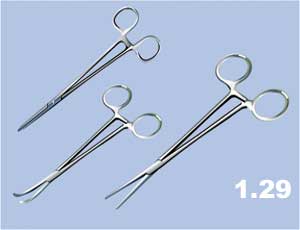
c) Hemostatic forceps or clamps look similar to needle holders and grasping forceps since they all have a pair of finger rings and a locking mechanism. Hemostatic clamps (forceps) can have straight or curved blades (Figure 1.29). They can be hard and forceful and able to crush tissue (crushing) or they can be soft in order to stop bleeding and not crush tissue (non-crashing).
i) Hard clamps. The most frequently used hemostatic clamps are called “snaps” or “Criles”. Other types include: “mosquitoes” which are light and small (Figure 1.30a); heavy arterial clamps (Kelly) (Figure 1.30b); and Lauer clamps (right angle) (Figures 1.31) that have an entirely curved tip. Mosquitoes and Kellies are used for permanent hemostasis of the bleeding points, with subsequent ligation of the bleeding vessel.

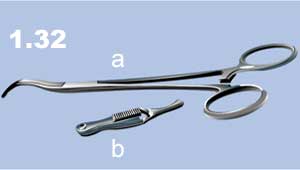
ii) Soft clamps. These are used to temporarily interrupt blood flow in a blood vessel. Figure 1.32a demonstrates a clamp used for a major vessels such as the aorta. Figure 1.32b shows a soft “bulldog” clamp used for medium-sized blood vessels. Hemorrhoidal or lung clamps (Figure 1.33) have triangular tips with serrated surfaces. They have strong grasping power and allow significant traction to be applied. These are commonly used on the heavy fascia.

d) Other types of forceps.
These include towel clips or towel-holding forceps with two sharp or flat ends which hold the edges of a towel in place (Figures 1.34a & 1.34b). Sponge-holding clamps (Figure 1.35) have large rings with serrated surfaces.



Retractors
Retractors are surgical instruments that are used to improve the visibility of the operating field by holding the tissue aside. There are many types of retractors.
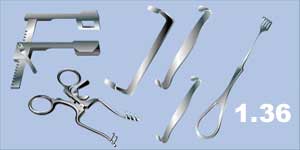
Figure 1.37 represents a plain retractor that has simple strips of metal fashioned into curves at each end (Parker).

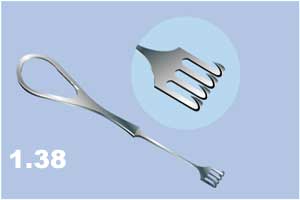
Rake retractors (Figure 1.38) have curved, blunt or sharp tips, and are commonly used for retracting skin edges.
Self-retaining retractors (Figure 1.39) have a simple locking mechanism that holds the retractor and the wound open without someone holding it.

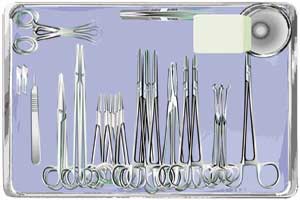
The diagram below demonstrates a surgical tray with additional instruments used for simple surgical procedures.
References #
- Agur AMR: Grant’s Atlas of Anatomy. Williams and Wilkins 9 th ed, Philadelphia. Pp650
- Anderson RM, Romth F: Techniques in Use of Surgical Tools. Appleton and Lange, Norwalk, Connecticut: 1990:pp211
- Annunziata CC, Drake DB, Woods JA, Gear AJ, Rodeheaver GT, Edlich RF. J Emerg Med. 1997 May-Jun:15(3);351-6
- Annunziata CC, Drake DB, Woods JA, Gear AJ, Rodeheaver GT, Edlich RF. Technical considerations in knot construction Part I – continuous percutaneous and dermal suture closure. J Emerg Med. 1997 May-Jun:15(3);351-6
- Aston SJ: The choice of suture material for skin closure, J Dermatol Surg 1976:2(1);57-61
- Athanasiou KA, Niederauer GG, Agrawal CM. Sterilization, toxicity, biocompatibility and clinical applications of polylactic acid/polycolic acid copolymers. Biomaterials. Jan 1996:17(2);93-102
- Atkinson LJ, Fortunato N: Barry and Kohn’s Operating Room Techniques. Mosby 8 th ed, 1999:pp988;163-295
- Boltri M. Atraumatic closure of skin wounds with fasterzip. Immediate and long term esthetic results. Minerva Chir. 1997 Nov:52(11);1405-9
- Borkaw A, Ellwood L. Planning for pediatric laceration repairs. Nurse Prac. 1996 Mar:21(3);42,45,49
- Casha JN, Hadden WA. Suture reaction following skin closure with subcuticular polydioxanone in total knee arthroplasty. J. Arthoplasty. 1996 Oct:11(7) ;859-61
- Charbit Y, Hitzig C, Bolla M, Bitton C, Bertrand MF. Comparative Study of Physical properties of three suture materials: silk, e-PTFE (Gore-Tex) and PLA/PGA (Vicryl). Biomed Instrum Technol. 1999 Jan-Feb:33(1);71-5
- Cnota MA, Aliabadi-Wahle S, Choe EU, Jacob JT, Flint LM, Ferrara JJ. Development of a novel synthetic material to close abdominal wall defects. Am Surg. 1998 May:64(5);415-8
