Description #
This unit is intended for healthcare professional to learn and practice the intramuscular injections.
Learning Objectives #
At the end of the units, students will be:
1. Familiar with the techniques for Intramuscular injections
2. Able to perform Intramuscular injections
Definition and Purpose:
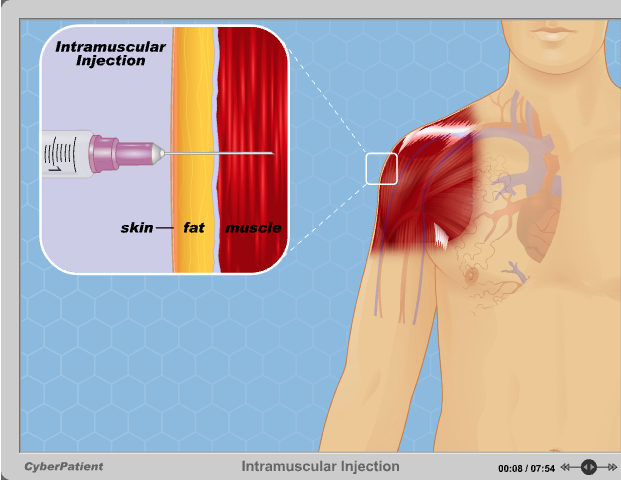
Intramuscular or IM injection is the injection of a substance directly into a muscle. In medicine, it is one of several alternative methods for the administration of medication.
Intramuscular injection is used for the delivery of certain drugs not recommended for other routes of administration, for instance intravenous, oral, or subcutaneous. The intramuscular route offers a faster rate of absorption than the subcutaneous route, and muscle tissue can often hold a larger volume of fluid without discomfort. In contrast, medication injected into muscle tissues is absorbed less rapidly and takes effect more slowly than medication that is injected intravenously. This is favourable for some medications.
Description #
Intramuscular (IM) injections are given directly into the central area of selected muscles. There are a number of sites on the human body that are suitable for IM injections; however, there are three sites that are most commonly used in this procedure.
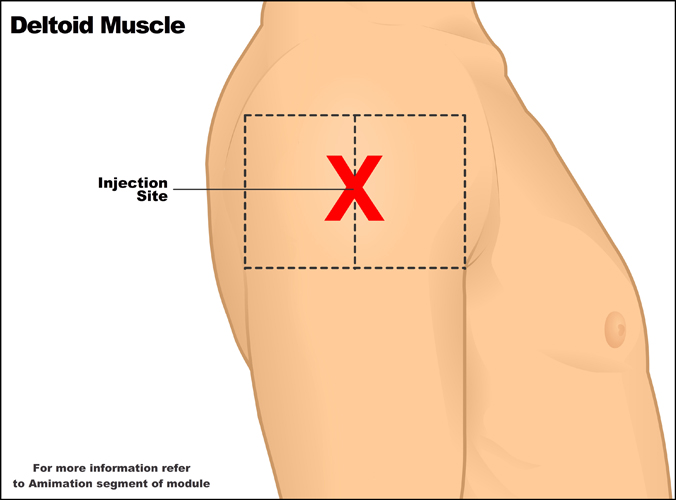
Deltoid muscle #
The deltoid muscle located laterally on the upper arm can be used for intramuscular injections. Originating from the Acromion process of the scapula and inserting approximately one-third of the way down the humerus, the deltoid muscle can be used readily for IM injections if there is sufficient muscle mass to justify use of this site. The deltoid’s close proximity to the radial nerve and radial artery means that careful consideration and palpation of the muscle is required to find a safe site for penetration of the needle. There are various methods for defining the boundaries of this muscle.
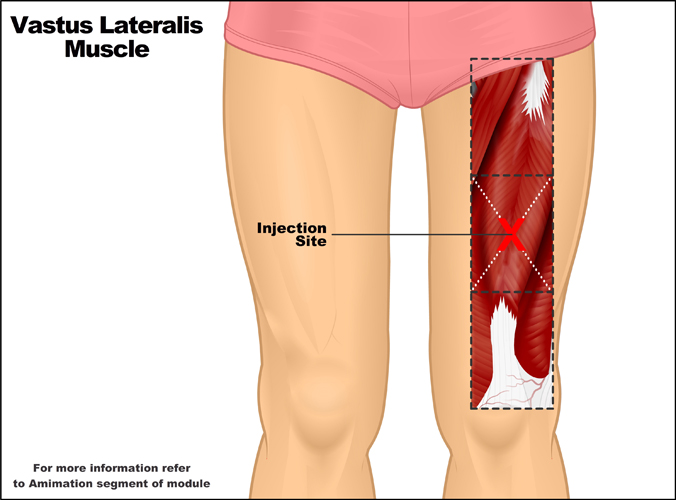
Vastus lateralis muscle #
The vastus lateralis muscle forms part of the quadriceps muscle group of the upper leg and can be found on the anteriolateral aspect of the thigh. This muscle is more commonly used as the site for IM injections as it is generally thick and well formed in individuals of all ages and is not located close to any major arteries or nerves. It is also readily accessed. The middle third of the muscle is used to define the injection site. This third can be determined by visually dividing the length of the muscle that originates on the greater trochanter of the femur and inserts on the upper border of the patella and tibial tuberosity through the patella ligament into thirds. Palpation of the muscle is required to determine if sufficient body and mass is present to undertake the procedure.
Gluteus medius muscle #
The gluteus medius muscle, which is also known as the ventrogluteal site, is the third commonly used site for IM injections. The correct area for injection can be determined in the following manner. Place the heel of the hand of the greater trochanter of the femur with fingers pointing towards the patient’s head. The left hand is used for the right hip and vice versa. While keeping the palm of the hand over the greater trochanter and placing the index finger on the anterior superior iliac spine, stretch the middle finger dorsally palpating for the iliac crest and then press lightly below this point. The triangle formed by the iliac crest, the third finger and index finger forms the area suitable for intramuscular injection.
Determining which site is most appropriate will depend upon the patient’s muscle density at each site, the type and nature of medication you wish to administer, and of course the patient’s preferred site for injections.
 Precautions #
Precautions #
Careful consideration in deciding which injectable route is to be used for the prescribed medication is essential. The intramuscular route should not be used in cases where muscle size and condition is not adequate to support sufficient uptake of the drug. Intramuscular injection should be avoided if other routes of administration, especially oral, can be used to provide a comparable level of absorption and effect in any given individual’s situation and condition. Intramuscular injections should not be given at a site where there is any indication of pain.
Complications and Contraindications #
Most complications of intramuscular injections are a result of the drug injected and not the procedure. However, it is possible that localized trauma of the injection site may result as part of the process. Minor discomfort and pain is common for a short period following the injection, but usually resolves within a few hours.
When the gluteal muscles are used, injections should be made on the upper, outer quadrant of the buttock to avoid damaging the sciatic nerve.
Injection fibrosis is a complication that may occur if the injections are delivered with great frequency or with improper technique.
Thrombocytopenia (low platelet count) and Coagulopathy (bleeding tendency) are contraindications for intramuscular injections, as they may lead to hematomas.
Preparation and aftercare #
Before administering medication, a health care practitioner verify the medication order for accuracy and prepare the medication from the vial or ampule.
- First, ensure you have identified the patient and assist them into a position which is comfortable and practical for access to the injection site you have chosen.
- Locate the correct area for injection using guidelines or skills taught during medical training. Clean the site with an alcohol swab or other cleansing agent.
- Prepare the syringe by removing the needle cover, inverting the syringe, and expelling any excess air. Approximately 0.1–0.2 ml of air should be left in the syringe so that the air in the top of the syringe chamber, when the syringe and needle are pointing down, forces the entire amount of medication to be delivered. This also prevents medication residue from being left in the needle, where it can leak into the subcutaneous and dermal layers when the syringe and needle are removed from the muscle.
- When ready to inject, spread the skin using the fingers of the non-dominant hand. Holding the syringe with the thumb and forefinger of the dominant hand, pierce the skin and enter the muscle. This process should be done quickly with sufficient control so as to lessen the discomfort of the patient. If there is little muscle mass, particularly in infants or the elderly, then you may need to pinch the muscle to provide more volume of tissue in which to inject.
- Aspirate at the injection site (while syringe and needle are within the muscle) by holding the barrel of the syringe with the non-dominant hand and pulling back on the syringe plunger with the dominant hand. If blood appears in the syringe, it is an indication that a blood vessel may have been punctured. The needle and syringe should be immediately withdrawn and a new injection prepared. If no blood is aspirated, continue by slowly injecting the medication at a constant rate until all medication has been delivered.
- Withdraw the needle and syringe quickly to minimize discomfort. The site may be briefly massaged, depending on the medication given. Some medication manufacturers advise against massaging the site after injection, as it reduces the effect and intention of the medication by dispersing it too readily or over too large an area. Manufacturers’ recommendations should be checked.
- Discard the used syringe and needle intact as soon as possible in an appropriate disposal receptacle.
- Check the site at least once more a short time after the injection to ensure that no bleeding, swelling or any other signs of reaction to the medication are present. Monitor the patient for other signs of side effects, especially if it is the first time the patient is receiving the medication.
- Document all injections given and any other relevant information.
Aftercare:
Monitor for signs of localized redness, swelling, bleeding, or inflammation at injection site. Observe the patient for at least 15 minutes following the injection for signs of reaction to the drug.
Animation* #
IM medications #
Examples of medications that are sometimes administered intramuscularly are:
- Codeine
- Morphine
- Methotrexate
- Metoclopramide
- Olanzapine
- Streptomycin
- Diazepam
- Prednisone
- Penicillin
- Sex hormones, such as Testosterone, Estradiol Valerate, and Depo Provera
- Dimercaprol
- Ketamine
- Lupron
- Naloxone
- Quinine, in its gluconate form
- Vitamin B12, also known as cobalamin
In addition, some vaccines are administered intramuscularly:
- Gardasil
- Hepatitis A vaccine
- Rabies vaccine
Influenza vaccines based on inactivated viruses are commonly administered intramuscularly, although there is active research being conducted as to the best route of administration.
Certain substances (e.g. Ketamine) are injected intramuscularly for recreational purposes.
Health care team roles #
The health care provider is obliged to undertake the following when administering an intramuscular injection:
- Inform and educate the patient on the need and effect of the medication being delivered.
- Ensure the correct identification and verification procedures are followed.
- Provide privacy for the patient during the procedure.
- Understand the theory behind selecting appropriate injection sites.
- Demonstrate correct technique when undertaking the procedure.
- Monitor for complications.
- Document all relevant information and ensure safe disposal of equipment.
