Description #
This unit will describe the correct administration, scoring and interpretation of the HOOS for THA patients.
Learning Objectives #
By the end of this unit, the learner will be able to perform the following tasks for THA patients:
– Administer the HOOS
– Score the HOOS
– Interpret the HOOS
#
What is this test? #
What is the HOOS? #
The Hip disability and Osteoarthritis Outcome Score (HOOS) is a valid3,4, reliable1,4, and responsive3 measure for assessing THA patients and falls within the WHO’s ICF domains of Body Function and Activity6 (Figure 1). The HOOS assesses pain, other symptoms such as stiffness, function in daily living (ADLs), function in sport and recreation (Sport/Rec), and hip related quality of life (QoL) over the past week1,2,4. Since it is a comprehensive test, it will take ~15-20 minutes for it to be completed and scored4.
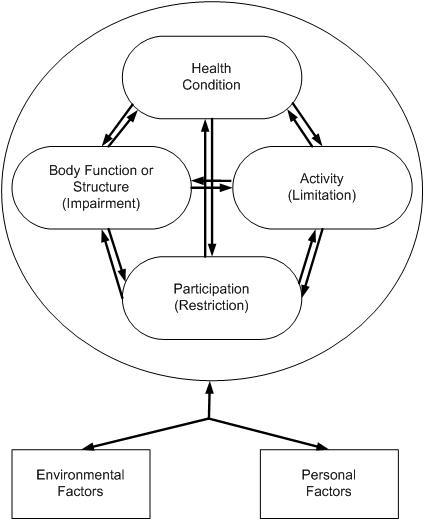
Figure 1. The International Classification of Functioning, Disability and Health (ICF) Conceptual Model. Taken from Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. Figure 2-17.
When do I use it? #
When do I use the HOOS? #
The Hip disability and Osteoarthritis Outcome Score (HOOS) can be used in a number of phases along the TJA Continuum of Care. Specifically, as seen in Figure 2, the HOOS is recommended for use in the Pre-Operative, Post-Acute, and Active Living phases of the TJA continuum. Health professionals can therefore use this outcome measure to monitor change in the patient’s status as he or she moves through these phases of the care (*note that it is not recommended in the Acute phase).
Figure 2. The phases along the TJA Continuum of Care for which the HOOS is recommended.

Equipment needed? #
What equipment is used to complete the HOOS? #
The equipment that is required will depend on how you have the patient complete the HOOS. If internet access is not available either at your clinic or the patient’s home, the patient will require:
- A paper copy of the HOOS which can be found here → Link to the Paper Version of the HOOS
- A pen
If your clinic or the patient has internet access, then an electronic version of the HOOS is available for the patient to complete at the link below.
Please bookmark the link on your web browser so you can access the HOOS quickly whenever you need it.
NOTE!
- While the HOOS is lengthy, as it requires the patient to respond to 40 questions, its value lies in its ability to capture many aspects of the patient’s experience (i.e. symptoms/stiffness, pain, function, sport, and quality of life).
How do I do it? #
How do I administer the HOOS? #
Since this is a patient reported outcome measure there is very little that you need to do. Just ensure that the patient has access to the paper or online version of the HOOS and have them follow the instructions at the top of the page. When they are finished, it will then need to be scored.
- Are you interested in learning more about the HOOS? If so, visit the official HOOS website to learn more!
How do I score it? #
How do I score the HOOS? #
Scoring the Hip disability and Osteoarthritis Outcome Score (HOOS) is easy to do:
- If the patient has completed the paper version of the HOOS, a spreadsheet for scoring is available at www.koos.nu.
- If the patient has completed the electronic version of the HOOS, then it will be automatically scored for you.
- Just in case you have not bookmarked the electronic version of the HOOS in your internet browser yet, the link to it can be found below.
Link to the Electronic Version of the HOOS
Data Tips! #
What do I do when items have been incorrectly marked or left blank on the HOOS? #
In some instances, your patient may have incorrectly marked or left items blank on the HOOS. Not to worry! The authors of the HOOS have compiled some examples of patient errors and how best to address them.
If the patient1:
- places a mark outside the check box. → Choose the box closest to the mark.
- marks two boxes instead of one. → Choose the box that indicates the more severe problem.
- answered < 50% of the subscale items in an individual subscale. → Then the individual subscale is considered invalid and no score should be calculated from that subscale.
- answered > 50% of the subscale items in an individual subscale → Then the subscale is considered valid.
To calculate the subscale score when > 50% of the items in an individual subscale are answered, you must calculate the mean score (average) within the subscale. If you are using the Excel spreadsheet provided at the HOOS homepage, then this will be automatically calculated for you. If you are using a paper copy of the HOOS, then take a look at the Example subheading under Data Tips! for guidance.
The minimum number of items completed for each subscale are as follows:
- 5 or more items from the Pain subscale must be answered
- 3 or more items from the Symptoms subscale must be answered
- 9 or more items from the ADL subscale must be answered
- 2 or more items from the QoL subscale must be answered
- 2 or more items from the Sport/Rec subscale must be answered
Example #
Example #
Mr. S is awaiting a right THA and has come to you for rehab prior to surgery. You choose the HOOS as your PROM and give it to Mr. S to complete. Mr S returns the HOOS and when reviewing the Symptoms subscale (Figure 3) you see the following:
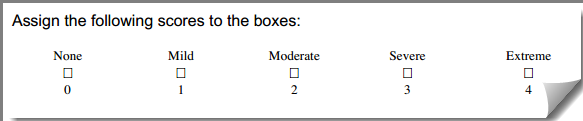
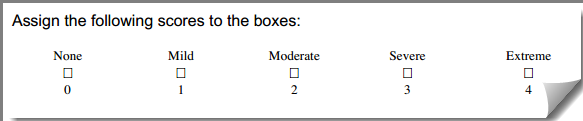
Figure 3. The Mr. S’s Symptoms subscale of the HOOS. Modified from www.koos.nu

Figure 4. HOOS Scoring Instructions.
Taken from Hip disability and Osteoarthritis Outcome Score (HOOS) Scoring Instructions
Please answer the following questions:
- What is the correct answer for S2.?
- What is the correct answer for S3.?
- What is the score for the Symptoms subscale?
Answers:
1. What is the correct answer for S2.?
Answer: Moderate. If a mark is placed outside a box, the closest box is chosen.
2. What is the correct answer for S3.?
Answer: Severe. If two boxes are marked, the box which indicates the more severe problem is chosen.
3. What is the score for the Symptoms subscale?
Answer: 42.
How did I get it?
1. Determine the values for each items in the subscale using Figure 4.
S1. = no answer
S2. = 2
S3. = 3
S4. = 2
S5. = no answer
2. Use the following equation:
Subscale Score = 100 – [(x/y)/4]*100
Where
- x = the total of the completed item values added together
- y = the number of completed item responses in the subscale
= 100 – {[(x)/y]/4}*100
= 100 – {[(2+3+2)/3]/4}*100
= 100 – {[7/3]/4}*100
= 100 – {2.333/4}*100
= 100 – {0.583}*100
= 100 – 58.3
= 41.7
= 42 (rounded)
What does it mean? #
How do I interpret the HOOS? #
It is simple to interpret the Hip disability and Osteoarthritis Outcome Score (HOOS) – the higher the score, the better. For example, a score of 100 in each subscale indicates no hip-related problems while a score of 0 indicates extreme hip problems. In addition, changes in the subscales can assist you in identifying if there has been CLINICALLY MEANINGFUL CHANGE. For example:
MCII is 24 in patients one year post THA for the pain subscale5
- What does this mean for my patient? It means that the change in score between test occasions must be greater than or equal to 24, in the pain subscale, in order for patients to experience a beneficial change that is clinically meaningful.
MCII is 17 in patients one year post THA for the QoL subscale5
- What does this mean for my patient? It means that the change in score between test occasions must be greater than or equal to 17, in the QoL subscale, in order for patients to experience a beneficial change in their quality of life that is clinically meaningful.
Are you interested in learning more about the HOOS? Please go to the official HOOS website to learn more!
Example #
Mr. S is a patient who initially saw you two weeks post op for his right THA. A year has now passed since his surgery and you would like to know if your treatment has produced a beneficial and clinically meaningful change. You have used the HOOS as your PROM and found the following information listed in Table 1:
Table 1

Using the information in Table 1 and Table 2, please determine if a beneficial and clinically meaningful change has occurred in each of the HOOS subscales.
Table 2
Has a beneficial and clinically meaningful change occurred in the Pain subscale? #
1. Calculate the change in score between test occasions
87.5 – 17.5 = 70.0
2. Compare the MCII to the change in score
70.0 > 24
Yes, a beneficial and clinically meaningful change did occur, as the difference in score between test occasions is greater than the MCII of 24 for the pain subscale.
Has a beneficial and clinically meaningful change occurred in the QoL subscale? #
1. Calculate the change in score between test occasions
81.25 – 12.5 = 68.75
2. Compare the MCII to the change in score
68.75 > 17
Yes, a beneficial change that is clinically meaningful did occur, as the difference in score between test occasions is greater than the MCII of 17 for the QoL subscale.
References #
- Website with users guide: www.koos.nu/
- www.orthopaedicscore.com/scorepages/hip_disability_osteoarthritis_outcome_score_hoos.html
- Nilsdotter A-K, Lohmander LS, et al. Hip disability and Osteoarthritis Outcome Score (HOOS) – Validity and responsiveness in total hip replacement. BMC Musculoskel Disorders 2003;4:10.
- Nilsdotter A, Bremander A. Measures of hip function and symptoms. Patient Outcomes in Rheumatology, A Review of Measures. Arthritis Care Res 2011;63(S11);S200.
- Paulsen A, Roos EM, et al. Minimal clinically important improvement (MCII) and patient acceptable symptom state (PASS) in total hip arthroplasty (THA) patients 1 year postoperatively. Acta Orthopaedica 2014;85(1):39-48.
- WHO International Classification of Functioning, Disability, and Health – http://www.who.int/classifications/icf/icf_more/en/
- Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. F.A. Davis Company: Philadelphia.
