MESP Umbilical Cord Prolapse Home Page #
Learning Objectives #
1. Describe the difference between cord prolapse and cord presentation.
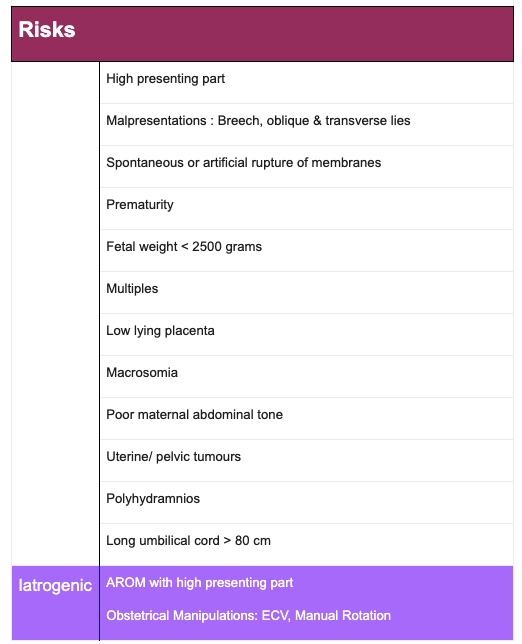
2. Identify risk factors associated with cord prolapse.
3. Outline essential actions to improve perinatal outcomes in the event of a cord prolapse.
Definitions #
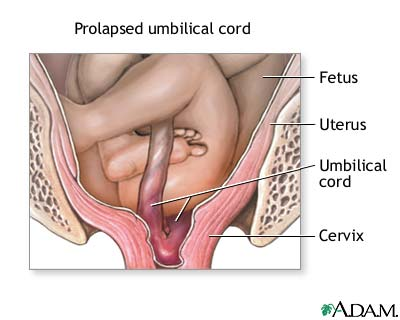
Umbilical Cord Prolapse occurs when the cord slips down alongside or ahead of the fetal presenting part.
Overt Cord Prolapse occurs when the cord advances in front of the fetal presenting part, usually through the cervix, into the vagina and sometimes outside the body. The amniotic membranes are ruptured and the cord can be seen at the introitus or felt on vaginal examination.
Occult Cord Prolapse occurs when the cord slips down alongside, but not beyond, the presenting part.
Cord Presentation occurs when the cord lies ahead of the presenting part in the presence of intact membranes.
Incidence:
The incidence of Cord prolapse is reported to be between 0.1 – 0.6 percent of all births. Cord prolapse is most likely to occur when the fetal presenting part is unengaged or non cephalic and the membranes rupture.
Diagnosis #
Confirmation of a cord prolapse / presentation may be made on vaginal exam. Cord prolapse can also be easily confirmed when the cord is visible at the introitus.
A sudden abnormal FHR is an indication for a vaginal exam to rule out cord prolapse, especially following rupture of the membranes. An occult prolapse poses a challenge in diagnosis but should be suspected if the FHR deceleration is sudden and prolonged.
Complications #
Cord prolapse is an obstetrical emergency. The fetus may experience hypoxemia, asphyxia and eventually death if the cord compression is not relieved immediately.
Cord compression is highly likely in the event of a cord prolapse. Cord compression can lead to umbilical vessel vasospasm and the obstruction of blood flowing in both directions between the placenta and the fetus.
The short-term impact of cord compression is the development of respiratory acidosis. Occlusion of the umbilical arteries reduces the blood flow bringing carbon dioxide to the placenta. This results in the build up of carbonic acid and the increase in hydrogen ion concentration (drop in pH). Carbonic acid is volatile and can be converted easily to water and carbon dioxide. It can occur quickly and resolves quickly with adequate gas exchange via the placenta in utero or lungs following birth.
A long term or abrupt and complete cord compression can also contribute to significant hypoxia and hypoxemia. By obstructing the blood flow through the umbilical vein there is a decreased supply of oxygen rich blood from the placenta to the fetus. After prolonged cord compression oxygen saturation falls and anaerobic metabolism becomes essential for cell function. A byproduct of anaerobic metabolism is lactic acid. Lactic acid takes a long time to create and a long time to clear. HCO3 buffers the increase in hydrogen ion concentration and the result is metabolic acidosis.
Cord compression and the Fetal Heart Rate: Cord compression occurs frequently in labour and is typically evident by the occurrence of abrupt drops in the fetal heart rate from the normal baseline and the abrupt return of the FHR to that baseline after a short interval lasting usually less than one minute. Any prolonged or profound cord compression will result in abnormally deep, complicated and prolonged decelerations of the FHR.
A cord prolapse often results in a sudden, prolonged fetal heart-rate deceleration, which may have been preceded by moderate to severe variable decelerations after a previously normal tracing.
On Intermittent Auscultation (IA) the fetal heart rate will likely be abnormal.
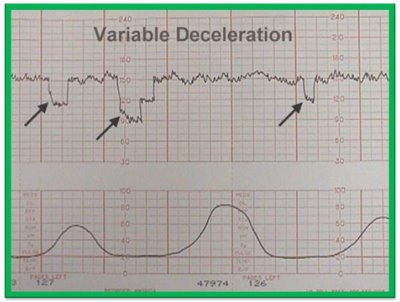
On Electronic Fetal Monitoring cord compression is associated with variable decelerations. With increasing and prolonged compression the fetal heart pattern will likely produce complicated variables, prolonged decelerations and eventually bradycardia if the compression is sustained.
A cord prolapse is usually a sudden event seen with rupture of membranes or a rapid dilation of the cervix with an unengaged or non-cephalic presenting part.
Risks #
Other conditions that present similar FHR characteristics include maternal hypotension, placental abruption, uterine rupture, and vasa previa, rapid fetal descent and Imminent birth with nuchal cord.
The cord may be palpable on vaginal examination or felt by the woman if the prolapse is overt.
Prolapse can occur at any cervical dilation, but is most common at 5–6 cm with the presenting part above spines.
Vaginal birth is seldom possible, except in the case of a fully dilated parous woman who can be supported to give birth rapidly within minutes of the cord prolapse. If that is the judgment of the midwife, then immediate action to accelerate the birth should be initiated.
If a vaginal birth is chosen:
- immediately encourage an upright position for gravitational aid,
- facilitate active pushing,
- cut a generous episiotomy,
- apply a vacuum if this is in your skill set and
- apply perineal pressure to accelerate the birth.
- consider delayed cord clamping. The newborn will likely be hypovolemic. Resuscitating the newborn with an intact cord will help correct the hypovolemia.
In the absence of the high likelihood of immediate birth, it is critical to immediately resuscitate the fetus in utero by decompressing the cord and arrange for emergency CS.
Management of Cord Prolapse #
The fetus needs immediate rescue
This can be accomplished successfully with immediate action.
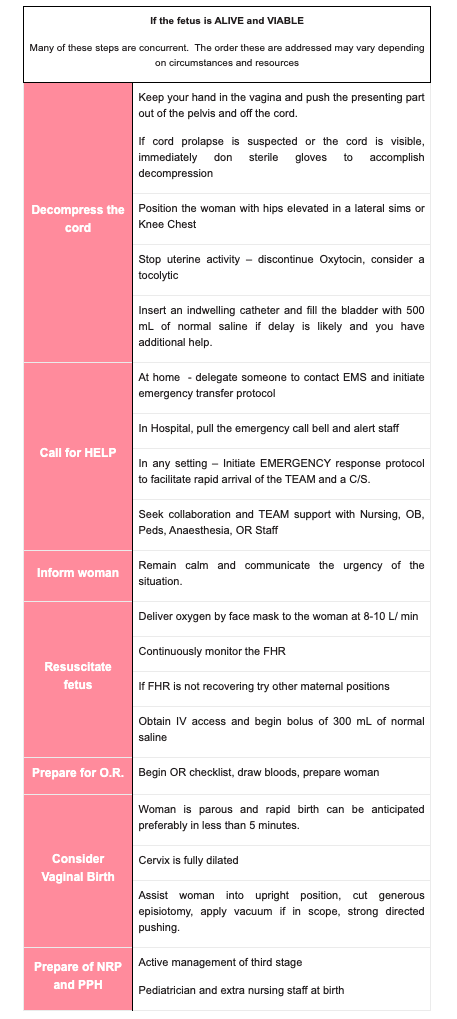
As long as the cord compression has been relieved the fetal circulation is restored the emergency is managed effectively for transfer. When cord compression was relieved and cesarean sections was undertaken within 30 minutes of diagnosis the neonatal outcomes have been good (Lin, 2005).


Management of Cord Presentation #
Cord presentation may be a chance finding on vaginal exam. As the membranes are intact there may be cushioning of the cord. Variable decelerations are likely to be found on EFM.
Management of Cord Presentation:
Cord presentation can be diagnosed prenatally by ultrasound. Vaginal birth is contraindicated and an elective CS should be arranged.
If you find a cord presentation on vaginal exam in labour
- remove your fingers immediately to prevent rupturing the membranes.
- Inform the woman and support her to assume a knee chest position.
- Seek immediate transport to the hospital, call EMS, notify your consultant OB and nursing staff to prepare the OR.
- Initiate continuous fetal monitoring, and prepare the woman for CS as in cord prolapse.
Material Resources Reading List
Select an item from the list below to download.
Sohrabi Davood, M.H. Karimfar and Asadi Fardin Department of Histology and Embryology, Department of Anatomy, Department of Pediatrics, University of Medical Sciences, Zanjan, Iran
