Basic Physical Examination Video #
Advanced Physical Examination Video #
Cardiac Assessment Unit: Basic Review #
Physiology
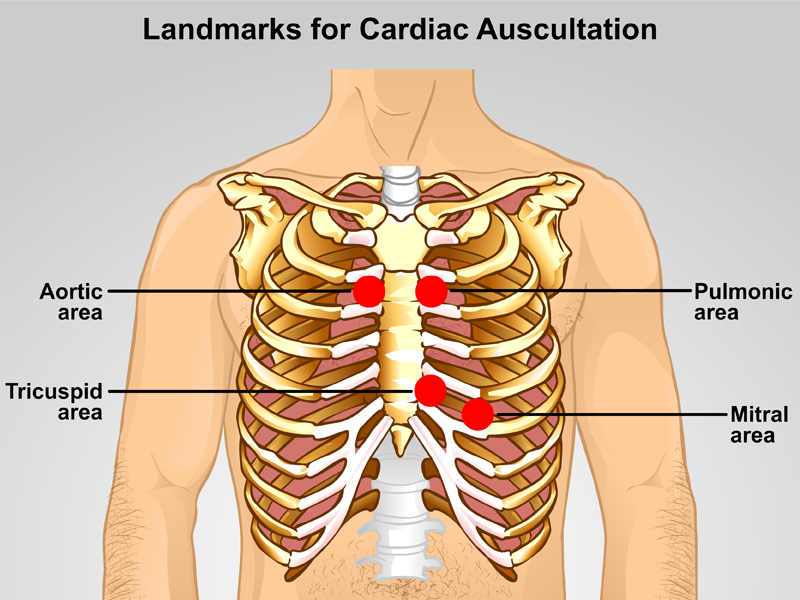
Landmarks for Cardiac Auscultation
Blood Flow
Cardiac Cycle
Heart Rate
Relationship between BP & HR
Health history
Physical Examination
Inspection
Palpation
Auscultation
Physiology #
Landmarks for Cardiac Auscultation
Blood Flow*
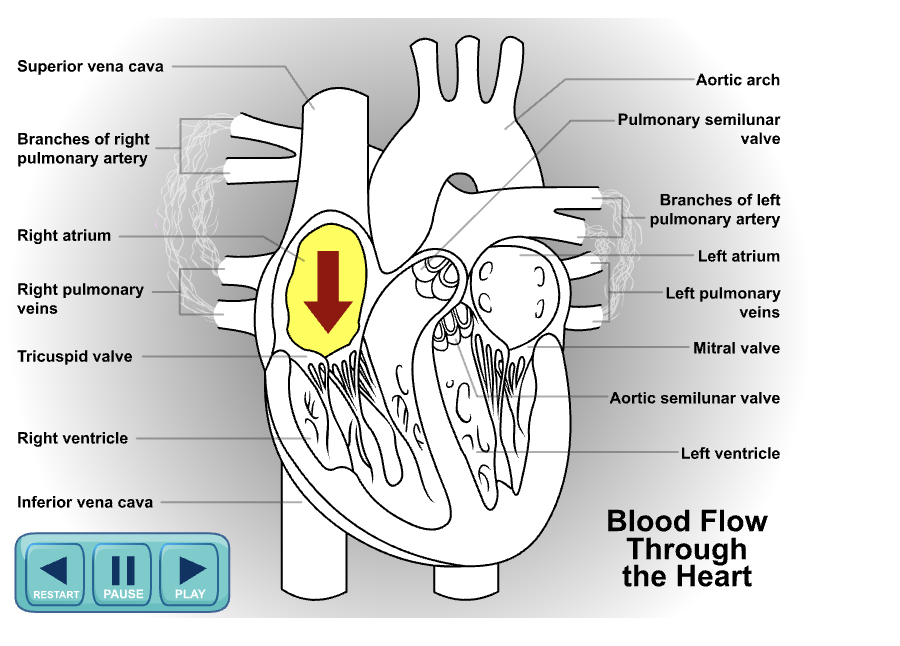
Cardiac CycleThe heart is a muscle pump which pumps blood through the body at a rate of 5-6 L/min. Although most diagrams show blood flow in one direction, one must note that both right and left side of the heart contract at the same time and not in sequence. What this means is that at any one point in time, oxygenated blood and deoxygenated blood is pumping through the left and right side of the heart in synchrony.
Heart RateThe heart rate is influenced by the ‘signal centers’ of the heart and each ‘centre’ has an inherent rate. Normal heart rate of an adult is between 60-100bpm.
The inherent heart rate of the
- Sinus node (heart’s pacemaker) is 60-80 bpm
- Atrioventricular node is 40-60 bpm.
Relationship between BP and HRHeart rate has a direct relationship with the blood pressure and reflects cardiac output (functioning of the heart). Four factors influences cardiac output (CO). They are preload, afterload, myocardial contractility and heart rate (Groer, 2001).
In review of the equations below, when the CO is low, the heart will compensate by increasing its heart rate to maintain optimal CO. As a consequence, the blood pressure increases until the compensatory mechanism fails. Once the compensatory mechanism ‘fails’, the BP and HR will drop as commonly observed with a client who is actively bleeding.
• CO = SV x HR
• BP = SVR x CO
SV (Stroke Volume)
- SV is the volume of blood pumped out by a ventricle with each beat and is dependent on ventricular contraction
- Determined by the Frank-Starling mechanism which affects EDV, thus preload
CO (Cardiac Output)
- CO is the amount of blood pumped out by each ventricle in 1 minute.
Tissue perfusion such as how well the kidney is perfused can be predicted with the use of MAP.
• MAP = D + (S-D)/3 or ((2xD) +S)/3
MAP (Mean Arterial Pressure)
- MAP is the “ pressure that propels the blood to the tissue throughout the cardiac cycle” (Marieb, 1992, p640) so it can indicate indirectly kidney function (perfusion of kidneys).
- Pulse pressure = (S-D)
S (Systolic pressure)
- Pressure exerted by blood on the blood vessel walls during ventricular contraction
D (Diastolic pressure)
- Drop in aortic pressure during diastole where the aortic semilunar valve is closed preventing blood from flowing back into the heart.
BP (Blood Pressure)
- Expressed as millimeters of mercury (mmHg)
- Typically refers to systemic arterial blood pressure in the largest arteries near the heart
HR (Heart Rate)
- Beats per minute
Health History #
With any physical assessment, one starts with a comprehensive health history if time allows. Otherwise, a concise list of questions specific to the cardiac system can be asked to elicit pertinent and relevant information which will guide you with your physical assessments.
Following are examples of questions one can enquire and explore with a client:
- Any history of MI or heart condition?
- Have you had any pain or pressure in your chest, neck or arm?
- Are you short of breath on exertion? How much exertion is necessary?
- Have you ever been woken at night short of breath?
- Can you lie flat without feeling breathless?
- Have you had swelling of your ankles?
- Have you noticed your heart racing or beating irregularly?
- Do you have pain in your legs on exercise?
- Do you have cold or blue hands or feet?
- Have you ever had rheumatic fever, a heart attack, or high blood pressure?
With any symptoms reported by a client, one needs to explore the characteristics of each symptom in detail in order to rule out potential causes. The following is one of the popular mnemonic many clinicians use for assessing symptoms: OPQRST
O nset
P recipitating factor(s)
Q uality
R adiating (location)
S everity (setting)
T emporal (duration?, changes in symptom? Associated symptoms?)
Using the above mnemonics, one can formulate systematic questions re: symptoms reported by a client. For example, with chest pain, the following questions correspond to the OPQRST mnemonic.
- When did the pain start?
- What brings on the chest pain? With activity? At rest? What kind of activities?
- How would you describe your chest pain?
- Where is the chest pain?; Where does the chest pain radiate to?
- On a scale of 0-10, 10 being the worst pain, where would you rate it? What number on the scale would be tolerable (allow you to do your activities of daily living) for you in terms of the pain?
- How long does the chest pain last? Is it constant? Does it come with other symptoms like SOB or dizziness? Is the chest pain the same as previous episodes or has it changed in characteristics?
With the cardiac system, chest pain is a primary symptom often reported by a client. However, one must understand that there are many underlying causes to chest pain and that 2/3 of all myocardial infarction/ischemia are silent (McGillion, 2006). “Silent” episodes mean the clients do not experience chest pain during a myocardial infarction/ischemia. Myocardial infarction/ischemia can only definitively be diagnosed through a 12-lead ECG and blood work (Troponin levels).
Physical Examination #
In context of the cardiac system, only 3 of the physical assessment techniques are relevant and necessary. Inspection, auscultation, palpation are required while percussion does not provide informative data to the nurse. There is controversy with regards to whether percussion is necessary in terms of cardiac assessment.
Equipment:
A stethoscope typical has a diaphragm and a bell. The diaphragm is best for high pitch sounds (e.g. apical heart rate and breath sounds) while the bell is best for low pitch sounds such as heart murmurs.
Inspection
During the Inspection phase, one is visually inspecting the following:
- Respiration rate (RR) and quality (shallow, deep, using accessory muscles?)
- Color of skin, mucous membranes, lips, and fingertips
- Presence of clubbing in digits
- Capillary refill (both fingers and toes)
- Presence of edema (pitting or non-pitting in lower and upper extremities and sacral area)
- Presence and quality of pedal pulses
- O2 saturation (ensuring that oximeter is functioning optimally by comparing displayed heart rate with actual apical heart rate)
*** Typically, inspection and palpation are done at the same time.
Palpation
During the palpation phase, one is simply assessing for warmth of the skin and extremities. In advanced assessment skills, cardiac thrills and heaves can be palpated by simply placing one’s hand (palm down) over the left side of the chest with one’s heel directly over the sternal border. For the actual technique of palpating for cardiac thrills, review the video on advanced techniques.
Auscultation
During the Auscultation phase, one is listening with a stethoscope for heart sounds. Heart sounds reflect the closure of heart valves. Basically, the “lub” and “dub” corresponds to S1 and S2 respectively. S1 indicates the closure of the atrioventricular valves–mitral (bicuspid) and tricuspid valves– while S2 indicates the closure of the semilunar valves–pulmonic and aortic valves. As such, S2 is auscultated clearly at the base of the heart while S1 is auscultated clearly at the apex of the heart.
It is good practice to auscultate the apical heart rate for one full minute to check for regularity, rate and quality (loud or distant). The apical heart rate provides informative data to you in determining the condition of the heart and should be checked pre and post cardiac medications such as digoxin.
With specialized units such as CCU or cardiac surgery, auscultation of the heart valves may be a part of one’s practice. The mneumonic APE- T o- M an (Aortic, Pulmonic, Erbs point, Tricuspid, Mitral) can assist one to remember the valves. For landmark placements, please refer to the landmark diagram previously posted. N.B. The position of the valve auscultation reflects the actual direction of sound conduction of the valves and does not reflect the actual position of the valves.
Acute Myocardial Infarction #
Acute Myocardial InfarctionThis site has detailed information for AMI
http://en.wikipedia.org/wiki/Myocardial_infarction#History
Definition:Acute myocardial infarction (AMI): An MI occurs when there is a blockage of the coronary artery resulting in necrosis of the cells of an area of the heart muscle and oxygen deprivation. (Melander, 2004)
Pathogenesis:Rarely does an MI occur in the absence of coronary artery narrowing. Infarctions are usually the result of an obstruction. During AMI, blood flow is diminished to the heart and depending on the extent of heart muscle affected, effects vary. Patients with severe MI will have decreased ejection fraction (amount of blood pumped from the heart with each beat). Reduced ejection fraction means decreased cardiac output which directly affects BP and pulse (refer to the section “relationship between BP & HR”) and so vital signs will be affected. Perfusion of organ will also be affected and result in decreased urinary output which can be estimated with the MAP. (Melander, 2004)
NTG is a vasodilator that increases venous capacitance by relaxing vascular smooth muscles thus reducing blood pressure by generalized vasodilation. The overall result is decreased preload and peripheral resistance which will help relieve chest pain.
Symptoms:Symptoms can vary with each patient and between genders. Patient may describe symptoms of “crushing pain” “indigestion” or “burning sensation”. The pain can radiate to back of chest, down the arm, up to the jaw. Pain does not alleviate with NTG. Other symptoms include uncomfortable pressure, crushing, heaviness, tightness, diaphoresis, nausea, and aching. Again, please consider that 2/3 of myocardial infarction are ‘silent’.
Physical Exam:Refer to previous section titled “Physical Assessments”
Sudden weight gain of > 1 kg overnight usually indicate fluid gain and may indicate inefficiency of the heart in pumping.
Puffy and swollen lower legs bilaterally due to fluid shift into interstitial space
Crackles to lung fields indicate fluid in lungs related to ineffective pumping of the heart (function is depending on condition of heart muscle)
Laboratory Findings:Troponin levels of > 0.3ng/ml
ECG – ST segment changes
Typical Medical Intervention post MI:
Heparin or enoxaparin (low molecular weight heparin) as per ordered by physicians to anticoagulate patient and thus reduce risk of thrombus formation. During AMI, there is a hypercoagulability that leads to blood cells to clump together which increases the closure of arteries and lead to a more severe MI (Melander, 2004).
PTT and INR levels are monitored for therapeutic levels of IV heparin.
Not responsibility of RNs to interpret ECG except within critical care areas
