Description #
Breech presentation is reported in 20-25% of pregnancies at the end of the second trimester and falls to 3-4% by term. Vaginal breech birth is associated with increased perinatal risk.
Ideally the presentation of the fetus is confirmed prior to the onset of labour which allows the primary care provider time to consult with an obstetrician and provide women with the information they need to make informed choices around options for birth.
Midwives are required to consult a physician when the fetus remains breech at 37 weeks gestation to ensure offering options for version and birth.
Although antenatal diagnosis is ideal, some breech presentations are not identified until labour and may happen during a planned homebirth or in the event of undiagnosed twins. Midwives must be prepared to assist in the birth of the breech infant. This unit reviews evidence and techniques that may be helpful to inform the care of the woman with breech presentation.
Learning Objectives #
1. Describe the three main breech presentations and their implications for vaginal birth.
2. Review the evidence for mode of birth in the presence of a breech presentation at term.
3. Describe the mechanism of labour in breech birth.
4. Outline the SOGC recommendations for offering vaginal breech birth.
4. Describe the steps for safely assisting at an undiagnosed out of hospital breech birth.
Breech #

Definitions #
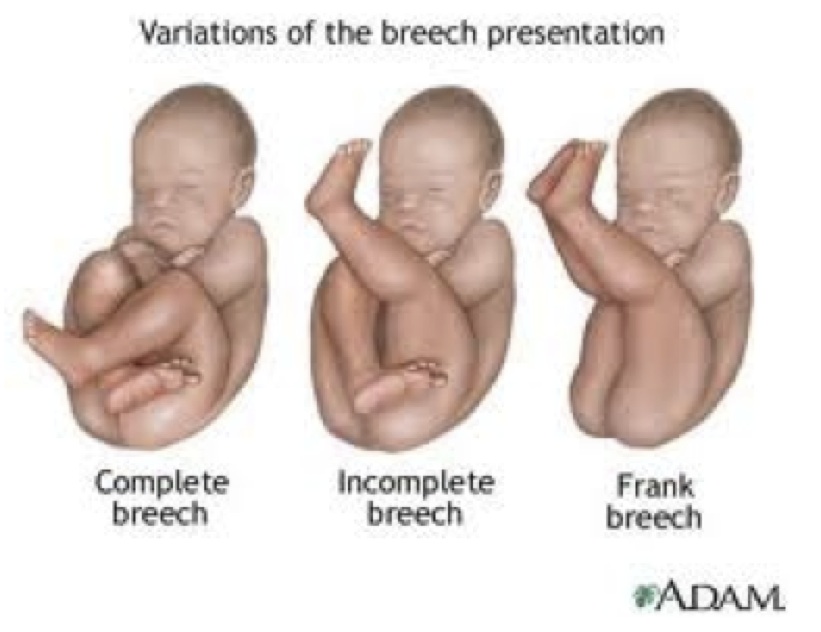
Breech presentation occurs when the caudal pole of the fetus presents first, with feet, knees or buttocks. It is the most common of the non-cephalic presentations
Complete Breech
The fetus is squatting or sitting cross-legged on the cervix with the knees flexed above the hips.
Frank Breech
The fetal buttocks enter the pelvis; hips are flexed, legs extended, and the feet by the baby’s head. The extended legs make it difficult for the baby to somersault to vertex, and often he remains lodged in the frank breech position. The extended legs also make external cephalic version more difficult. Frank breech accounts for about half of all breech presentations and is most favorable for a vaginal delivery as there is little opportunity for cord prolapse in this position
Footling Breech[
One or both hips and knees are extended and one or both feet are presenting. A variation of this is the kneeling breech. This risk of cord prolapse and entrapment of fetal parts is highest with this presentation.

Incidence
Rates of breech presentation decrease as gestational age advances. At 28 weeks gestation the fetus is breech 20-25 % of the time, but by term the rate has fallen to 3-4% (SOGC, 2009). Twenty-five percent of fetuses who are breech at 36 weeks will spontaneously turn to cephalic presentation before labour (Hofmeyr, 2007).
Associated Conditions & Risks #
Conditions associated with Breech Presentation
These conditions can contribute to breech presentation
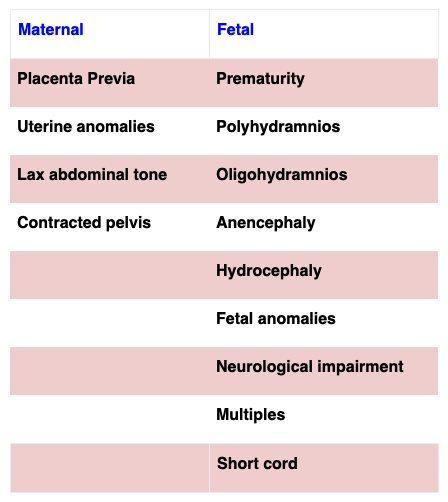
Compared to cephalic presentations, the woman and breech fetus are at increased risk (Hofmeyr 2005).
The Risks Associated with Breech Birth include:

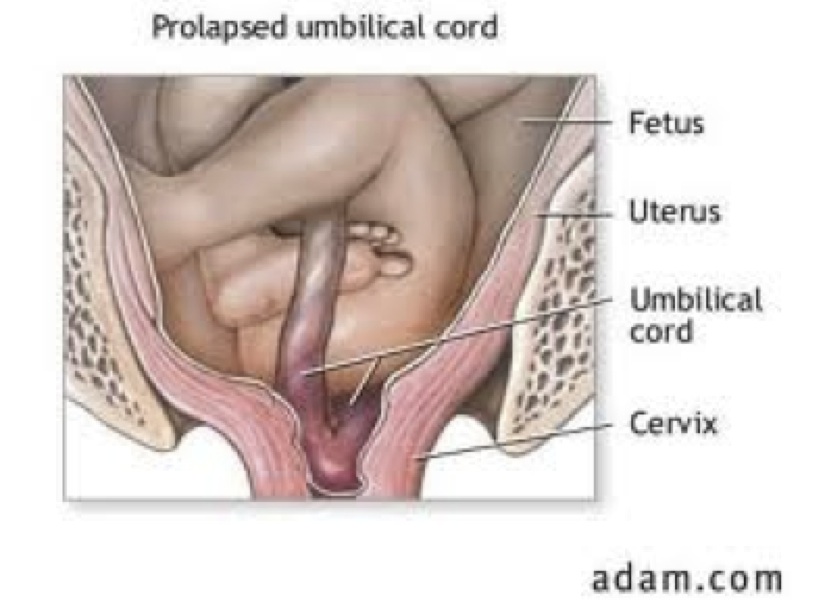
Cord Compression & Prolapse
The irregular shape of the non-cephalic presenting part can create gaps where the cord can slip through. A cord prolapse is significantly less common when the breech is frank.
Cord compression leads to hypoxia and can result in asphyxia, organ injury and death.
Entrapment of fetal parts
In a cephalic presentation the fetal head can mold and conform to the pelvis during the course of labour. In the breech there is no time for the head to accommodate the mid pelvis. The body and legs are born first, followed by the shoulders and the after coming head must come quickly after that.
It may not become apparent that the fetal head is not able to negotiate the pelvis until the body is born.
Extended arms above the head and or an extended fetal head (star gazing) can delay birth of the head – leading to fetal trauma, asphyxia and death.
The head of the preterm and asymmetrically growth restricted fetus is proportionately larger than the rest of the body.
Entrapment of the fetal head is a real concern if the body descends before the cervix is fully dilated or the head is disproportionately larger than the boney pelvis. This is most evident with the macrosomic infant or the asymmetrical IUGR fetus.
Intrapartum Trauma
Fetal trauma can occur through hyperextension of the fetal neck and manipulation of the fetal soft tissues.
Abruptio
Abruption can occur with rapid decompression of the uterus after birth of the torso before the birth of the head. This results in hemorrhage and fetal hypoxia
Hands off the Breech
Stimulating the fetus by handling or pulling on the emerging body can cause the fetus to extend its head or reach above its head with its arms. This can result in a birth delay with serious sequelae. Prolonged cord compression can contribute to asphyxia and death. Hyperextension of the fetal head creates a larger diameter entering the pelvis and can contribute to serious cervical spinal cord lesions (Gabbe, et al., 2007)
The Evidence on Mode of Birth #
The Term Breech Trial (Hannah et al 2000)
- A multicenter randomized clinical trial (RCT) involved 2,088 term fetuses in frank or complete breech presentations at 121 institutions in 26 countries.
- The trial was discontinued early due to an interim analysis that demonstrated an increased risk of adverse outcomes in newborns in the vaginal birth arm.
- The authors concluded cesarean delivery for term breech presentation significantly decreased perinatal and neonatal mortality and neonatal morbidity.
A five year follow up of that trial found no difference in infant death rates or neurodevelopmental delay by age 2 years but there was increased maternal morbidity in the C/S group (Whyte et al, 2004).
Critique of the Term Breech Trial
Several methodological issues have been identified that challenge the external validity of the Term Breech Trial (Kotaska, 2008).
- Investigators failed to eliminate cases where adverse outcomes were unrelated to birth route
- Serious neonatal morbidity was defined imprecisely.
- The selection process allowed twins, antepartum fetal demise, footling breech and hyperextened neck into the trial
- Inexperienced practitioners delivered a significant number of the babies with poor outcomes.
When corrected numbers are compared, the difference between groups appear no longer significant
The PROMODA study
Goffinet (2006) and colleagues conducted a prospective study at 175 centers in Belgium and France and reported on the outcomes from 8105 women who presented with a breech fetus at term. Of these term breech presentations 69% were delivered by C/S. A trial of labour (TOL) was offered to 31%. Vaginal breech births occurred in 71% of the TOL population and the overall vaginal breech birth rate from the 8105 woman was 22.5%. They reported on the same outcomes that were included in the Term Breech Trial and found no difference in perinatal mortality or serious morbidity overall. They did find a lower 5 minute Apgar in the TOL group (0.16%) compared to the C/S group (0.02%). The births were all attended by clinicians skilled in breech birth. They used a conservative approach. Every woman received an US prior to or in early labour and had continuous electronic fetal monitoring in labour. This data provided some confidence to offer select women an option to consider vaginal birth.
Loss of skill and experience with vaginal breech
The Term Breech Trial was published in 2000. In the ensuing years there have been several cohorts of North American trained obstetrical specialist who have completed their formal education without the opportunity to acquire the skills or experience to support a vaginal breech birth.
In 2009 the SOGC joined the ACOG and RCOG in advocating a trial of labour in an appropriate setting for select women with a singleton breech fetus at term. (SOGC, 2009)
The World Health Organization (WHO, ) recommends vaginal birth if the fetus is frank breech with a flexed head, the maternal pelvis is adequate for fetal size, and the woman has not undergone prior cesarean section for cephalopelvic disproportion. Because of the increased risks associated with breech birth, every breech delivery should occur in a hospital with surgical capability.
Optimal Characteristics to consider Vaginal Breech #
Ideal characteristic for vaginal breech birth:
- Frank or Complete
- > 36 weeks’ gestation
- a normal labor pattern
- no contraindications to vaginal birth.
- Estimated fetal weight 2,500–4,000 g,
- AGA
- head flexed
- Absence of anomalies that may obstruct delivery
- birth attendant skilled in breech birth,
- emergency cesarean readily available
- Informed choice: Women should be counseled on the risks and benefits of vaginal breech birth.
Breech at Term #
Assessing the Breech
Assessment of fetal lie and presentation is part of a routine prenatal examination toward the end of pregnancy and at the onset of labour. However, even skilled providers can report missing breech presentations on occasion.
On palpation, a breech is not as rigid as a fetal skull, and the groove that divides head from shoulders is absent. A fetal head can be balloted (bounced between the examiner’s thumb and fingers) in the fundus. Ballottement of the breech moves the baby’s body and is accompanied by more resistance. Breech presentation often causes maternal rib pain and lower abdominal cramping from the fetal feet kicking the bladder. The FHR may be auscultated the loudest in the upper quadrants.
On vaginal examination, the solid sacrum of a frank breech can feel like a skull, and in early labor a high station may confuse diagnosis. An edematous face presentation feels similar to the breech on cervical examination until the provider carefully assesses landmarks—the greater trochanters and anus form a straight line, whereas the malar bones and mouth form a triangle. With the breech, fetal genitalia may be palpable, and meconium may be present on the examiner’s finger. If a limb is felt alongside the presenting part, determine whether it is a foot or a hand. Sometimes ultrasound confirmation is necessary. If the lie is unstable near term or the provider is uncertain about presentation after 34–36 weeks an ultrasound examination is indicated.
Version #
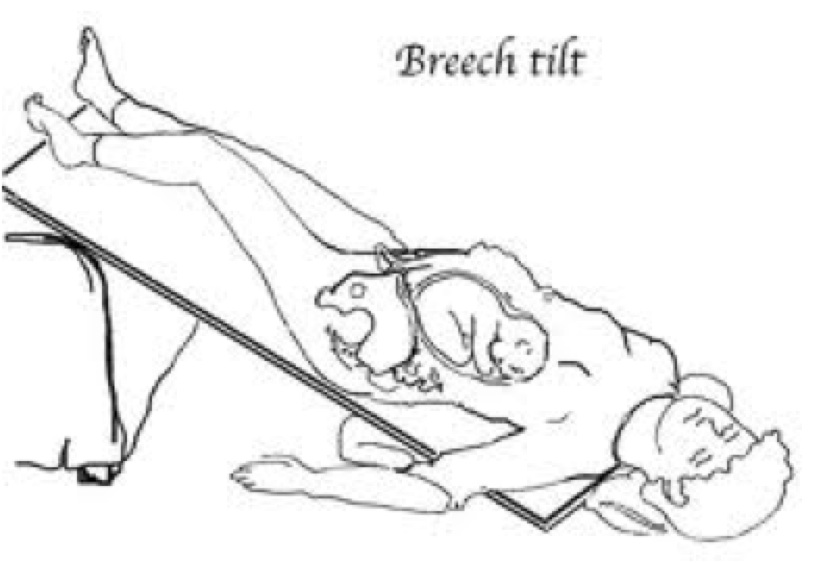
Postural positions
Knee chest and elevated hips has traditionally been recommended to facilitate spontaneous version prior to labour.
A Cochrane metanalysis of six studies involving 417 women with breech fetuses found no difference between the control and intervention groups in the rates for non-cephalic births, cesarean section and Apgar scores below 7 at one minute, even when ECV was also attempted (Hofmery, 2011)
Conclusion: There is insufficient evidence from well-controlled trials to support the use of postural management for breech presentation. The numbers of women studied to date remain relatively small. Further research is needed.
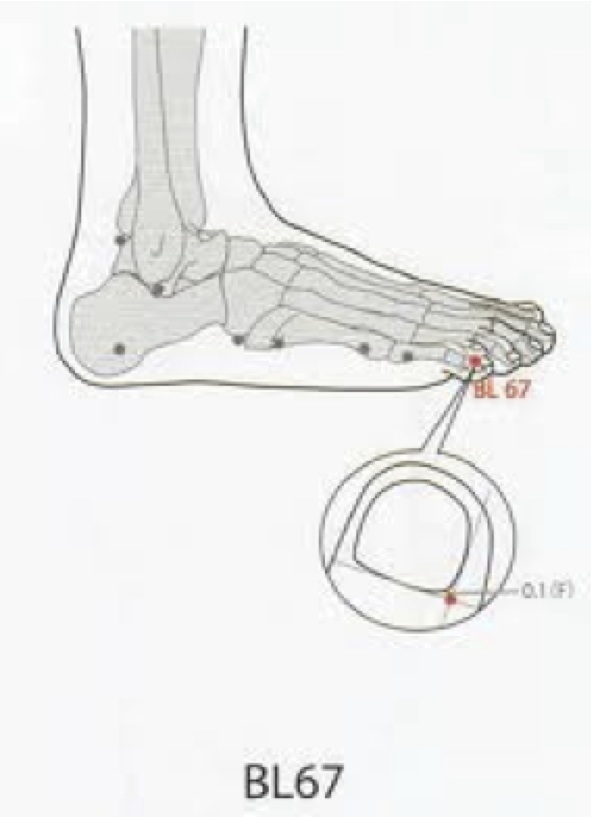
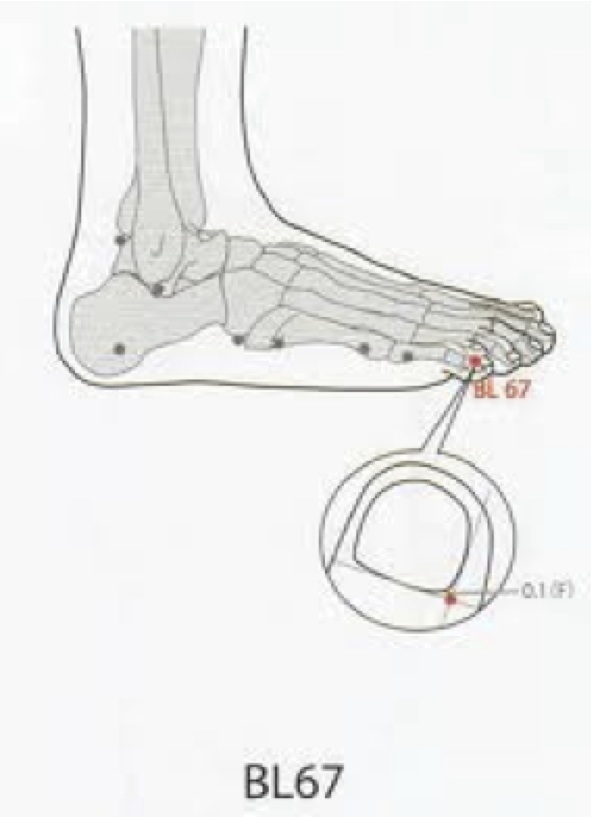
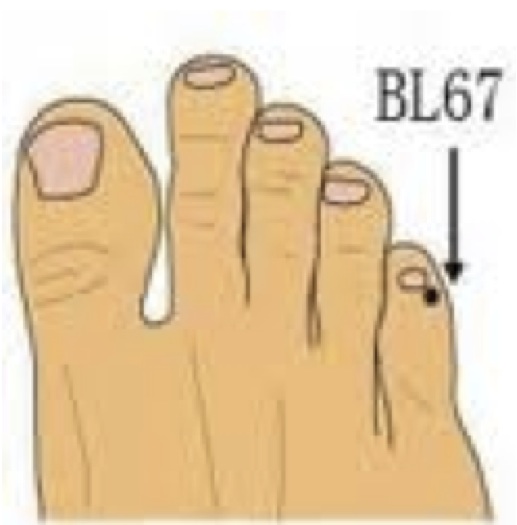
Acupuncture and Moxibustion have been used to turn breech babies.

A Cochrane metanalysis found a decrease in need for ECV and oxytocin use in labour with its use (Coyle, 2005; Cardini 1998; Cardini, 2005).
A RCT comparing acupuncture plus moxibustion to BL67 to placebo acupuncture reported an increase in cephalic presentation at term in the treatment group (Neri et al, 2004).
External cephalic version (ECV) is the trans-abdominal manual rotation of the fetus into a cephalic presentation.
ECV is recommended > 37 weeks if vaginal birth is not otherwise contraindicated as there is a clinically and statistically significant reduction in breech presentation and C/S and no difference in adverse perinatal outcomes (Hofmeyr & Kulier, 2011).
ECV prior to term may decrease the rate of breech and CS however, the differences were not statistically significant (Hutton, 2011).
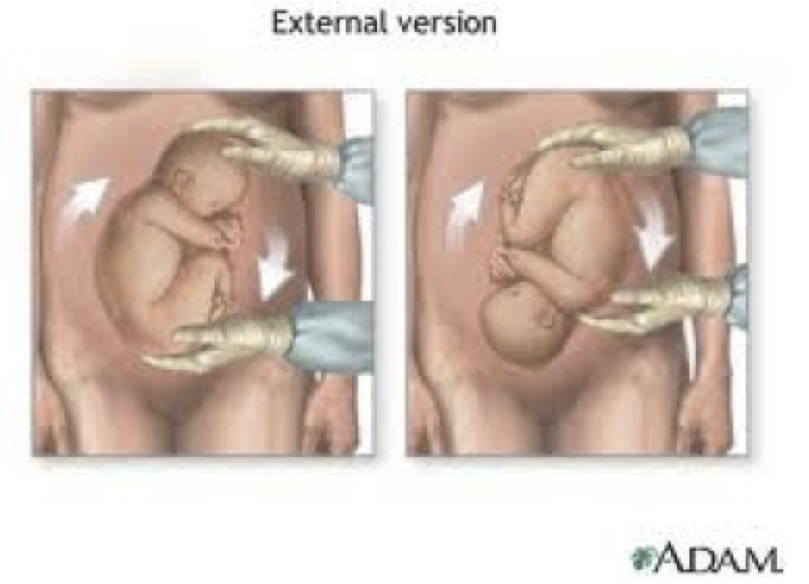
Complications resulting from ECV are rare and include:
- Fetal trauma,
- Rupture of membranes,
- Labour
- Cord prolapse or entanglement
- Placental abruption,
- Fetomaternal hemorrhage (0–5%),
- Abnormal FHR
Relative contraindications to ECV include active labor, uterine scarring, polyhydramnios, oligohydramnios, fetal growth restriction, uterine malformation, or fetal anomaly.
Techniques for Vaginal Breech Birth #
Mechanisms of Breech Birth
· The bitrochanteric diameter enters the pelvis in the transverse orientation, rotating in midpelvis and arriving at the pelvic outlet in the anterior-posterior position.

· After the buttocks deliver, the body rotates, usually with the back anterior, and the shoulders descend in the same way.
· The anterior shoulder delivers as the flexed head enters the pelvis in the transverse diameter.
· The baby rotates internally so that the chin appears at the perineum, then the face, followed by the rest of the head, which delivers by flexion.
The Centre for Excellence in Teaching and Learning (UK) – offer the Breech Birth (2007) tutorial. The learning tool outlines the movement of the breech through the pelvis and the hand manoeuvers used to assist with the birth.
UK Midwife Mary Cronk recommends the following rules be observed in attending a breech birth
• Don’t push a breech through a pelvis with oxytocic drugs
• No inductions, no augmentations
• If the labour does not progress – C/S
• Don’t pull a breech down through the pelvis – no breech extractions
• Breech by propulsion, not traction
• If it isn’t coming down – C/S
• Keep your hands off – sit on them if necessary
• Be ready to bag and mask.
Consideration for supporting vaginal breech birth:
- Adequate descent is determined if the breech is at the level of the ischial spines when the cervix is 6 cm dilated, and reaches the pelvic floor at full dilation.
- If the breech does not descend further with pushing efforts, cesarean section is usually necessary.
- Nulliparas usually give birth within 1 hour of active pushing, multiparas in about half the time.
- There are three positions to support a spontaneous breech birth. Semi Sitting, squatting and all fours.
Semi-sitting or Squatting
- Assist the woman to an upright, supported squat, or semi-Fowler’s at the edge of a bed.
- The woman may have a strong urge to push, but it is crucial that she refrain from pushing until she is fully dilated and the breech is very low. Even when fully dilated, passive descent of the fetus or open glottis pushing may be safer than vigorous pushing until the breech is on the perineum.
- Episiotomy, if required, is not performed until the fetal anus has appeared at the introitus.
- A hands-off approach encourages the fetal head to maintain a position of flexion during the birth. The sensation of being grasped can startle the emerging baby, causing his hands and arms to extend in a Moro “startle” reflex and potentially stimulate the baby to extend the neck or trap the arms above the head. This posture presents larger diameters of the head to the pelvis or wedges the arms up alongside the head.
General Guidance: HANDS OFF THE BREECH
- Unnecessary interference can cause serious injury to the infant, including organ damage and limb fractures. Breech extraction is associated with a birth injury rate of 25% and a mortality rate of approximately 10%, and should only be performed by obstetricians in the management of breech second twin (Fischer, 2006).
- There appears to be consensus to not touch the breech up until birth to the umbilicus – from that point forward there are two divergent opinions on what follows – 1) allowing the breech to hang vs 2) supporting the breech in the neutral position
- Some experts advocate wrapping the emerging infant in a warm towel or blanket to keep the baby warm. Cool air may cause hypothermia, and can stimulate breathing efforts with the head still unborn. Use warm hands or a warm towel.
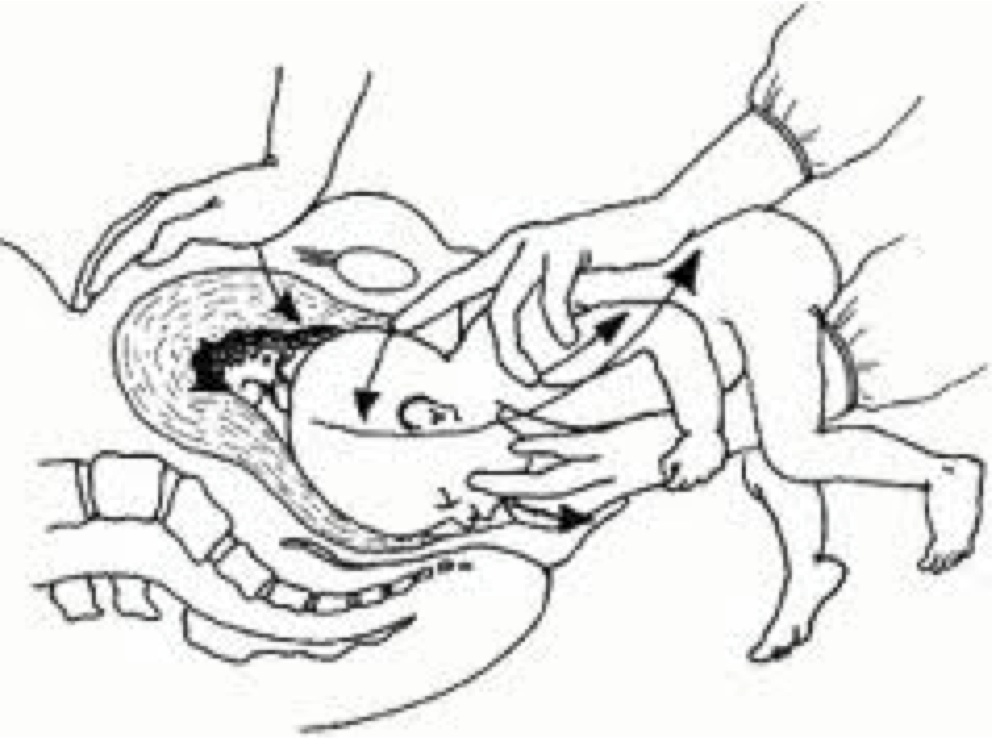
- Generally, only place your hands on the baby if absolutely indicated. If you must be hands on – refrain from touching the abdomen. Place your thumbs over the sacrum and your fingers of each hand around the iliac crest or along the femurs and hips (as in for the lovset manoeuvre).
The frank breech usually delivers with one hip toward the pubic bone and the other toward the mother’s sacrum, his back to either the right or left.
First the anterior hip delivers, then the posterior hip with lateral flexion, the body emerging to the umbilicus.
There is no evidence that pulling a loop of cord down to create slack is of any benefit, and in fact may cause spasm of the cord vessels (Howell et al, 2007)
Encourage the mother to push with contractions as this is a crucial point in the birth. At this stage, the head has entered the pelvis, and the cord is probably compressed between the pelvic bones and the baby’s head.
To reduce the risk of anoxia, many recommend the head be born within 4 minutes once the umbilicus is seen.
External rotation should occur until the baby’s back faces up, and you should gently guide the infant to a back- up position if he does not naturally achieve that on his own. Note placement of hands above.
Eventually, the feet should spring free as the body descends.

Modified Pinard
When the legs are extended and the progress appears delayed, the attendant may need to assist to release the legs.
If the legs appear trapped, place two fingers on the medial aspect of the thigh and splint the femur. Apply pressure along the inside aspect of the thigh and push the femur away from the midline at the hip joint. This also applies pressure to the popliteal fossa, facilitating the knee bending and the foot to come within reach so that the foot can be gently pulled down.
There are two schools on approach from this point on:
- Allow the breech to hang and keep your HANDS OFF the baby.
- Allow the breech to hang but keep your hands on the fetal pelvis to support the weight and take pressure off the cervical spine.
Wait until you see the scapula. If at this point the arms are extended, use Lovset Manoeuver to reduce the arms. In this manouver you are relieving an obstruction, not pulling the baby out.
With maternal pushing, the shoulders present in , or turn to, the anterior-posterior plane and emerge sequentially.
For the head to appear, the occiput must be low enough in the pelvis to hinge around the back of the symphysis.
- Some suggest at this point continue to let the breech hang.
- Others suggest supporting the body by placing an arm through the legs and along the abdomen.
Allow the head to descend through the pelvis until you see the hairline.
When the hairline appears, gently lift the fetal body upwards into a neutral position using the Mauriceua Smeilie Veit manoeuver.
Avoid hyperextension of the neck or excessive pressure on the cervical spine as this will occlude the vertebral arteries and can lead to necrosis of the cervical cord.
An assistant can apply suprapubic pressure directly behind the maternal pubic bone to keep the fetal head flexed and aid the birth.
The head should be born slowly. Instruct the woman to pant or blow while you assist the birth by flexion
In most cases, the head will spontaneously deliver.
Offer active management of third stage as the woman is at increased risk of PPH and you have increased likelihood of need to resuscitate the newborn.
Managing the undiagnosed breech at home: Semi sitting/ Squat
- Call EMS and initiate transfer protocol with your local hospital.
- Explain the situation to the woman, her family and your second attendant.
- Empty the bladder with a catheter
- Assist the woman into a position that allows the breech to dangle
- Discourage strong pushing until the breech is on the perineum.
- When the breech is on the perineum encourage strong pushing
- Allow the baby to deliver unassisted—hands off the breech
- Note time when body delivers to umbilicus, you have approximately 4 minutes
- Assist the legs if this is deemed necessary
- If there is progress, keep hands off
- Consider wrapping the baby’s emerging body in a towel and gently provide support
- Assist birth of the arms as necessary
- Encourage the back to rotate anteriorly
- When the baby’s hairline is seen, use the mauriceau smellie viet manouver
- Position his body on your forearm and place the fingers of your dominant hand on the fetal maxilla
- Place your opposite hand over the baby’s back with two fingers over his shoulders and middle finger pressing on the occiput
- Ask assistant to apply suprapubic pressure to assist with head flexion.
- Gently lift the baby to the horizontal plane to deliver the face with flexion from your fingers – have her pant or blow at this point to prevent rapid birth of the head.
- Prepare for postpartum hemorrhage and neonatal resuscitation
Managing delivery of the Breech on all fours – Hands and Knees

In recent years the hands and knees has been advocated as an alternative approach to support breech birth.
CLICK HERE to view a slide show of an illustrated Hands & Knees Breech Birth by Mary Cronk.
You can view a short video of a hands and knees breech homebirth. Scroll down slowly on the page linked here and select the video.
Note: We do not advocate planned homebirth for breech presentations.
The principles are the same.
HANDS OFF THE BREECH
- Call EMS and initiate transfer protocol with your local hospital.
- Explain the situation to the woman, her family and your second attendant.
- Empty the bladder with a catheter
- Assist the woman onto all fours
- Discourage strong pushing until the breech is on the perineum.
- When the breech is on the perineum encourage strong pushing
- Allow the baby to deliver unassisted—hands off the breech
- Note time when body delivers to umbilicus, you have approximately 4 minutes
- Assist the legs if this is deemed necessary
- If there is progress, keep hands off
- Assist birth of the arms as necessary
- To assist with birth of head you may press gently on fetal chest
- Keep hands near chest to support infant when head is born.
- Prepare for postpartum hemorrhage and neonatal resuscitation
Delayed Cord Clamping
We recommend delayed cord clamping to enable physiological transfusion from the placenta and cord to the newborn.
Active Management of the Third Stage of Labour (AMTSL)
Please offer AMTSL to all women. Consider recommending this approach in light of the potential increased risk of PPH and the likelihood of newborn transition issues.
Controlled birth of the after-coming head
- Mauriceau Smellie-Viet Manoeuver
- Piper forceps are used by obstetricians and can effectively achieve delivery of the head.

In the event of fetal head entrapment:
- Immediately insert your hand into the vagina and make an airway for the baby by keeping the maternal tissue away from the face.
- if indicated, thread oxygen tubing into the space you have created and supply supplemental O2
- Keep the cord warm and moist and avoid handling it.
- Wrap the fetal body in dry warm towels
- Establish IV access in the woman with a large bore catheter and infuse a crystaloid solution
- In low resource settings, symphysiotomy is sometimes performed.
- The Zavanelli maneuver can be used to replace the fetus into the uterus to be delivered by cesarean, but this technique carries a high risk of uterine rupture and fetal injury or death (Hofmeyr, 2007a).
If the cervix traps the head
- Dührssen incisions are sometimes made at the 2 o’clock or 10-o’clock position on the cervix to release the head. Extension into the lower uterine segment can occur and cause severe bleeding.
Lovset’s Manoeuver #
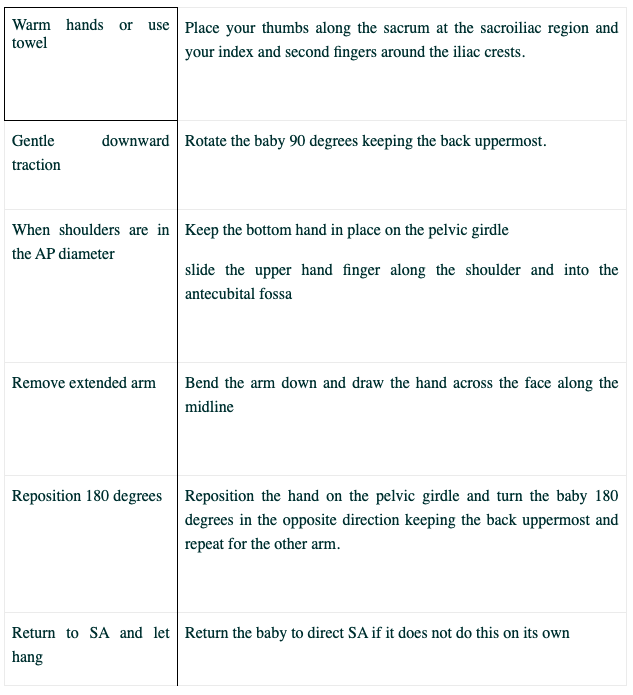
Click on the link here to view a diagram of Lovset Manoeuver

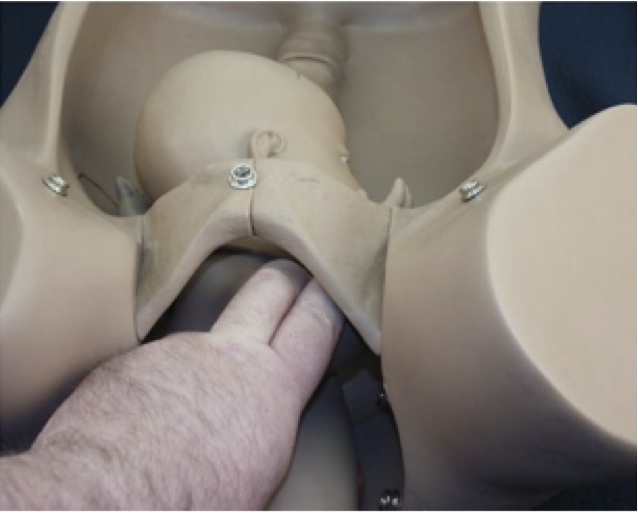
Mauriceau-Smellie-Veit manoeuver #
The Mauriceau Smellie Veit Manoeuver click here to see diagram
- Drape the baby’s body over one arm
- Place two fingers, one on each side, over the fetal malar eminence on the maxilla.
- use these fingers to pull the face forward in flexion.
- With your other hand, place the ring finger and index fingers, one each over the shoulders on the fetal back and place the middle finger on the fetal occiput.
- Use this finger to push the fetal head forward to support flexion.
- Flex the head with pressure from both hands. Avoid compressing the neck or inserting fingers in the mouth.
- An assistant may also do suprapubic pressure to assist with the power above to help birth the head and keep it flexed.
- Birth the head slowly.
- Instruct the woman to pant / blow while you assist the birth by flexion. The fetal chin, mouth, nose, eyes and forehead will sweep the perineum in that order before the fetal head emerges.
