Learning Objectives #
Review causes, diagnostics and treatment for bleeding in early and later gestation including:
– Miscarriage
– Hydatidiform mole
– Ectopic pregnancy
– Abruptio Placentae
– Placenta Previa
– Vasa Previa
Early Pregnancy Bleeding – Ectopic Pregnancy & Pregnancy Loss #
Antepartal bleeding – first half of pregnancy #
First-trimester vaginal bleeding occurs commonly in both viable and nonviable pregnancies. Twenty (20) to forty (40) percent of women experience bleeding during the first trimester, and many of these will give birth to healthy babies at term (Tulandi & Al-Fozan, 2006). Most bleeding in early pregnancy results from one of five causes. These causes are contained in the mnemonic TEMPT:
Threatened Abortion
Ectopic Pregnancy
Maternal pathology of uterus, cervix or vagina
Physiological
Trauma
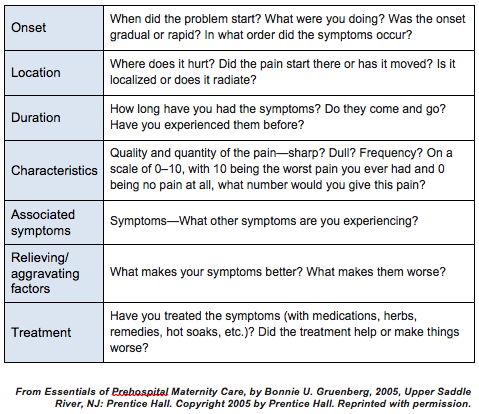
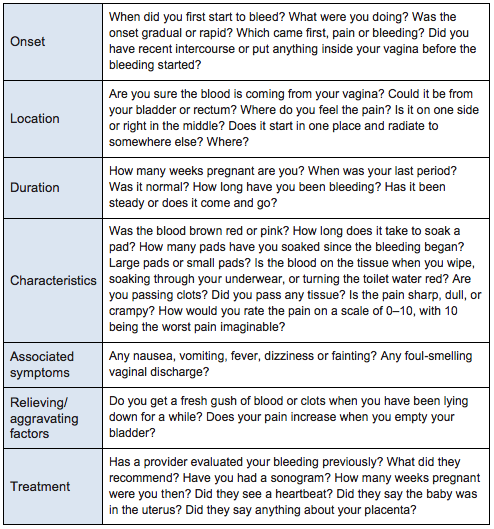
On presentation, a comprehensive history is important. The midwife should determine:
Possible Causes of Early-Pregnancy Bleeding #
- Threatened Abortion
- Lost fetus in multiple pregnancy
- Hydatidiform mole
- Ectopic pregnancy
- Maternal pathology of uterus vagina, or cervix
Polyp, cervicitis, cervical carcinoma
Cervical hemangioma
Condyloma, neoplasm, foreign body, laceration, ulceration
Infection—bacterial vaginosis, trichomonas, chlamydia, gonorrhea
- Physiological
Implantation bleeding
Cervical ectropion (columnar epithelium exposed by eversion of the endocervix)
- Trauma
Vaginal, cervical, vulvar laceration
Ectopic Pregnancy #
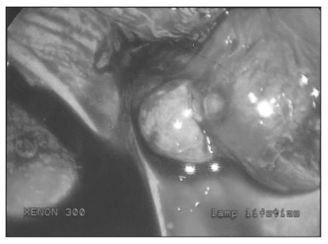
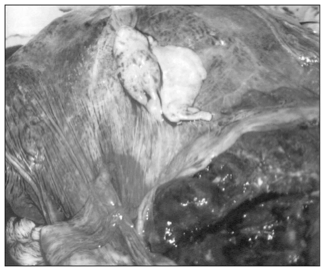
Ectopic (“out of place”) pregnancy occurs when the embryo embeds somewhere outside the uterus. The most common site is the fallopian tube (95%), but occasionally the embryo will implant on the ovary (4%), cervix (1%), or even in the abdominal cavity (<1%) (Tulandi, 2007a). None of these structures is suitable for supporting a growing embryo, and the fragile, vascular fallopian tube is vulnerable to rupture.
The incidence of ectopic pregnancy is between 1-2 % of all pregnancies. In the United States the occurence of ectopic pregnancy has tripled since 1970 to 1 in every 44 pregnancies.
Heterotopic Pregnancy is when there is one embryo in the uterus and one ectopic. It is exceptionally rare event (1 in 40,000) except in cases of assisted conception. They are very difficult to diagnose.
Ectopic pregnancy is the leading cause of first-trimester maternal death in Canada and 5th overall cause for any pregnancy related maternal death.
Normally, conception occurs in the fallopian tubes, and the conceptus reaches the uterus within about a week. There it encounters the thick, hormonally-primed endometrium and taps into the mother’s bloodstream for life support.
Ectopic pregnancy begins as clinically indistinguishable from intrauterine pregnancy (IUP), but in time it begins to distend the tube and invade blood vessels. Placental and corpus luteal function falter, and hormone levels begin to drop.
The decidua, no longer maintained by a healthy corpus luteum, begins to shed, causing bleeding. If the ectopic pregnancy ruptures the tube or erodes through the tube wall, the woman will hemorrhage into her abdominal cavity, potentially creating the hemodynamic equivalent of a shotgun blast to the abdomen.

In other cases, the ectopic pregnancy will die and spontaneously resolve, form a chronic hematoma, or abort out the end of the tube, sometimes reimplanting as an abdominal pregnancy. Rupture can initially present as a small defect in the tube with minimal pain and bleeding that grows gradually worse or as massive hemorrhage. Fortunately, using modern diagnostic techniques, most ectopic pregnancies may be diagnosed before they rupture.
The woman with an ectopic pregnancy may not realize that she is pregnant. Pain and bleeding usually appear between 6-10 weeks gestation. Symptoms can occur as early as 5 weeks’ gestation or (rarely) as late as 14–16 weeks (Tulandi, 2007a). Half of women with extrauterine pregnancy have no symptoms prior to tubal rupture and have no known risk factors (Tulandi, 2007a).
Signs and Symptoms
- The classic presentation of ectopic pregnancy is the woman with amenorrhea, abdominal pain and vaginal bleeding.
- Pain onset is abrupt, severe and is often unilateral; but in some cases, the woman may have chronic discomfort with irregular spotting for days before becoming acutely symptomatic.
- Rupture of the fallopian tube rapidly progresses to hypovolemic shock: rapid, weak pulse; confusion and restlessness; dizziness, pale, clammy skin; collapsed neck veins; hypotension; and syncope.
- Three of four women will have abdominal pain with rebound tenderness, rigidity, and distention. Rebound tenderness is sudden severe pain when the hand is rapidly released following abdominal palpation.
- Free blood in the abdomen may cause nausea, vomiting, and diarrhea and irritate the phrenic nerve, which runs under the diaphragm, causing referred pain to the right shoulder.
- Bimanual exam may elicit cervical motion tenderness 67% of the time(Sivalingam, 2011) an /or a palpable adnexal mass in approximately 50% of cases (Sivalingam, 2011).
- Blood pooling in the cul de sac may cause a sensation of rectal pressure.
- Cullen’s sign is rare: blue tint beneath the umbilicus indicates free blood in the abdomen
- Atypical presentation is common: 1/3 women have no signs and 9% have no symptoms – they may present with ambiguous signs and symptoms that mimic many other gyne problems (Sivalingam, 2011).
- MOST WOMEN WHO DIED were MISDIAGNOSED in the primary care or emergency care settings (Sivalingham, 2011)
Always consider ectopic pregnancy a possibility unless the conceptus has been sonographically confirmed in the uterus.
- Because the consequences of a ruptured extrauterine pregnancy can be so devastating, suspect ectopic pregnancy in any woman of reproductive age with lower abdominal pain, vaginal bleeding, and amenorrhea.
Abdominal pregnancy carries a high mortality rate for both mother (20%) and fetus (40–90%), and congenital deformities from compression are common (Tulandi, 2007a). The placenta attaches to the outer uterus, bowel, mesentery, liver, spleen, bladder, or ligaments and may separate anytime during pregnancy, causing uncontrollable hemorrhage. Oligohydramnios, poor placental definition, abnormal fetal lie, and an empty uterus low in the pelvis are visible on ultrasound, although late in gestation the thickened gestational sac may be misidentified as an IUP by an unsuspecting sonographer.
Risk factors for ectopic pregnancy include:
- Tubal disease, damage due to previous surgery (tubal, pelvic or abdominal) or infection (PID, chlamydia)
- Infertility
- Assisted reproductive technology
- Smoking (1/3 of all cases are associated with smoking, esp > 20 cig/day)
- Age > 35
- Contraceptive failure: progestin only pill or intrauterine device (IUD)
- Altered hormone levels
- Prior ectopic pregnancy
Differential diagnoses include
- spontaneous abortion,
- ruptured ovarian cyst,
- appendicitis,
- salpingitis (infection of the fallopian tube),
- torsion (twisting) of the ovary,
- round-ligament pain,
- torsion or degeneration of a uterine fibroid,
- kidney stone,
- abscess, and
- urinary-tract infection.
Diagnosis
Early diagnosis provides an opportunity for less invasive approaches to care and a decreased risk to the woman of tubal rupture.
Ectopic pregnancy is diagnosed by a combination of
- serial β-hCG concentrations and
- Transvaginal ultrasound
Transvaginal Ultrasound (TVUS) : High definition ultrasounds offer significant improvement in diagnosis especially by the transvaginal route. False positives can occur when an adnexal mass is actually corpus luteum, bowel, paratubal cysts, hydrosalpinx or an endometrioma. False negatives are possible if ectopic is small or concealed. It is possible for an ectopic to go undiagnosed on an Ultrasound.
- In a normal IUP a TVUS should confirm a gestational sac almost 100% of the time at 5.5 weeks.
- A yolk sac and cardiac activity should be visible by 6 weeks.
- Ectopic pregnancy can be diagnosed with the presence of adnexal mass and an empty uterus (sensitivity 84-90%; specificity 94-99%)
- Aproximately 8/10 ectopics are located on the side of the ovarian corpus luteum.
- Identification of an intrauterine pregnancy rules out ectopic pregnancy unless there is a heterotopic pregnancy.
- Pregnancy of Unknown Location (PUL) is reported when the US is unable to identify pregnancy location. An US that finds a PUL should be followed up with diagnostic pathways until the pregnancy location is determined.
Ultrasonographic findings helpful in the diagnosis of ectopic pregnancy (Sivalingham et al, 2011)
- Absence of intrauterine pregnancy
- Positive indication of an ectopic pregnancy mass: inhomogenous mass, empty adnexal gestation sac or adnexal sac containing yolk sac or fetal pole
- Free fluid: suggestive of ectopic pregnancy in the absence of IUP, but not diagnostic as a small amount may be physiologic
β-hCG concentrations: Normally, β-hCG levels will increase by AT LEAST 35-66% every two days in the first trimester. Failure of levels to rise in this fashion may suggest early pregnancy failure. A rapid drop in levels over 2 days by 21-35% indicates a spontaneous abortion or resolving ectopic. In Ectopic pregnancies the levels may either rise or fall. However, regardless of which direction they are going – most ectopic pregnancies will see a slower rise or decline than expected for an intrauterine pregnancy. An ectopic pregnancy is highly likely when the history is not compatible with a spontaneous abortion, or the β-hCG concentrations continue to rise when the pregnancy location by TVS remains unknown.
A Discriminatory β-hCG level is the serum concentration of β-hCG when a pregnancy is expected to be visible on Ultrasound Scan. Romero and colleagues (1985) reported that a discriminatory β-hCG level of over 6,500 iu/L had a sensitivity of 100% and a specificity of 96%, a positive predictive value of 87% and negative predictive value of 100% with abdominal U/S. Current levels for the discriminatory zone are reported between 1,000, 1500 to 2000 IU/ L (RCOG, 2004) with TVUS. The level is used will depend on the quality of the technology, the skill of the sonographer, prior knowledge of the woman’s risks and symptoms and anatomical factors such as the presence of fibroids and multiple pregnancy (RCOG 2004)
Serum Progesterone may be used although there is no definitive value that establishes an ectopic pregnancy from an intrauterine one. Serum progesterone in viable pregnancies are > 50 ng/mL.
Diagnostic Laparoscopy – may be indicated with inconclusive US and a suspicion of ectopic. However, ectopic pregnancies may still be missed with this approach.
N.I.C.E Public Information for women regarding ectopic pregnancy and miscarriage
Diagnostic Imaging Pathway for Suspected Ectopic Pregnancy
Important Points #
- Transvaginal and abdominal US combined with the measurement of serum β-hCG are the investigations of choice for suspected ectopic pregnancy
- In a small proportion of cases the TVUS may be non-diagnostic. Follow up of these patients is dependant on the value of the quantitative β-hCG –
- A β-hCG > 1500 IU should proceed to laparoscopy
- A β-hCG < 1500 IU should be repeated in 48hrs if the woman is clinically stable, expecting a rise of > 66%.
- A normal US does not exclude an ectopic pregnancy
Implantation bleeding #
Implantation bleeding occurs about 10–14 days after fertilization and is thought to be caused when the implanting embryo disrupts the blood vessels of the uterine lining.
Implantation bleeding results from vascular disruption as the embryo burrows into the endometrial tissue. Implantation bleeding can be scanty or profuse; it usually occurs 4–6 weeks after the last menstrual period and lasts a day or two. Due to its timing, some women who experience this may report this episode of bleeding as a period which in turn can contribute to inaccurate dating.
Threatened Miscarriage #
Miscarriage (formerly spontaneous abortion) #
Miscarriage is the most common complication of pregnancy. Approximately 1 out of 10 women with a positive pregnancy test will miscarry, 80% of these during the first trimester (Tulandi & Al-Fozan, 2006). By 16 weeks gestation the risk of miscarriage for normal fetuses decreases to 6 per 1,000 (Tulandi & Al-Fozan, 2006). Pregnancy loss, or threatened loss is a stressful event that should be handled with sensitivity and compassion. About 30-50% of women who experience vaginal bleeding in the first trimester will lose the pregnancy. The cause of miscarriage is frequently not clear. The risk increases with each consecutive miscarriage.
A threatened miscarriage (previously threatened abortion) occurs when bleeding or abdominal pain is accompanied by a closed cervix. An ultrasound may identify a fetal heartbeat, empty gestational sac, or an empty uterus if gestational age is very early. Most women with bleeding beyond 7 weeks’ gestation with documented fetal heart activity will not miscarry; however, first-trimester bleeding increases the likelihood of adverse pregnancy outcome, including growth restriction, preterm birth, and stillbirth, especially when the bleeding is heavy or extends into the second trimester.
In most cases, the bleeding results from a small abruption or subchorionic hematoma. Often this separation of the placenta from the decidua cannot be visualized on ultrasound. If the hematoma is visible and symptomatic, pregnancy loss is more likely. Incidental findings of small, asymptomatic subchorionic hematomas do not increase risk.
The most common cause of pregnancy loss is chromosomal abnormality: too many or too few chromosomes, defective or missing genes, or missing chromosomal segments. The majority of early miscarriages are autosomal trisomies (three copies of a chromosome), including trisomy 21 (Down syndrome), trisomy 18, and trisomy 13. Parents may carry a rearrangement of chromosomes (usually a translocation or inversion) or each parent may carry a harmless single copy of problematic gene that is lethal as a homozygous pair. Advanced maternal age increases the risk of pregnancy loss due to poor egg quality, a less receptive endometrium, and endocrine dysfunction. Embryos fathered by men with a high percentage of abnormal sperm are also less likely to survive.
Pregnancy loss may also be caused by toxins such as anesthetic gases, agricultural chemicals, cocaine, moderate to high alcohol consumption, and tobacco use, and by infections such as Listeria monocytogenes, Toxoplasma gondii, cytomegalovirus, and primary genital herpes. Urinary-tract infections are a risk factor for spontaneous abortion.
More than 10% of women with repeated pregnancy loss have congenital uterine anomalies that interfere with implantation or uterine distention, such as bicornuate or unicornuate uterus (Tulandi & Al-Fozan, 2007). Women with an untreated septate uterus have greater than 60% risk of pregnancy loss, probably because inadequate blood supply to the septum causes implantation failure (Tulandi & Al-Fozan). Submucous leiomyomas can also interfere with implantation, as can intrauterine adhesions and endometrial abnormalities that develop after pregnancy-related dilation and curettage (D&C) procedures.
Endocrine factors such as decreased thyroid function, inadequate progesterone production, and abnormal prolactin levels play a significant role in recurrent pregnancy loss. Poorly controlled diabetes with hA1C above 8% can cause congenital anomalies and both early and late pregnancy loss (Tulandi & Al-Fozan, 2007). The maternal immune system can cause pregnancy loss by attacking and killing the conceptus. Thrombophilias can cause clotting within spiral arteries and the intervillous space on the maternal side of the placenta, causing abnormalities of the uteroplacental circulation that can lead to pregnancy loss, intrauterine growth restriction (IUGR), abruption, or preeclampsia.
About one third of the miscarriages occurring before 9 weeks’ gestation are “blighted” or anembryonic (Tulandi & Al-Fozan, 2006). The gestational sac and placenta develop, but no yolk sac or embryo. On ultrasound examination, the gestational sac will be 20 mm or more, but no embryo will be visible. Severe bleeding, abdominal or back pain, passage of tissue, and cervical dilation indicate inevitable pregnancy loss. This condition progresses to either complete abortion or incomplete abortion. In early pregnancy, the woman may be given the option to complete the miscarriage naturally or consider a medical (misoprostol) or surgical (D & C) abortion to hasten the process and limit blood loss and pain.
Incomplete Miscarriage (formerly incomplete abortion) #
In incomplete miscarriage some products of conception are expelled while other parts, usually placental fragments, are retained in the uterus.
Usually the body will expel the products of conception without medical or surgical intervention when the pregnancy loss occurs early in the first trimester. In pregnancies that abort later in gestation retained placental tissue can cause significant bleeding that can result in hypovolemic shock. Women may experience intense pain. The cervix is usually dilated and tissue may be lodged in the cervical os. Beta-HCG levels are plateaued or slowly falling. An ultrasound will indicate retained products in the uterus or thickened, irregular endometrium (greater than 5 mm double stripe). In this case, a D&C is likely necessary to complete the process and stop the bleeding.
Missed Miscarriage ( previously Missed Abortion) #
In a missed miscarriage, the products of conception are retained in utero after the fetus has died. Expulsion occurs days or weeks later.
Signs & Symptoms
The nausea, breast tenderness, and urinary frequency of pregnancy may subside, and vaginal spotting may occur, though the cervix usually stays closed.
Diagnosis
Ultrasound detects no fetal heartbeat. BHcG levels will be falling and not consistent with gestational age.
Management
In early pregnancy, management can be expectant; but with advancing gestational age or prolonged retention of pregnancy, medical or surgical intervention is recommended.
Septic Miscarriage (previously septic abortion) #
In septic miscarriage, infection invades the uterine cavity during the abortion process.
Septic miscarriage may occur after conception with an intrauterine device (IUD) in place; with prolonged, undiagnosed rupture of membranes; or after interventive attempts to end a pregnancy – most often in the absence of skilled hands, and lack of adherence to aseptic technique.
Signs & Symptoms
- fever,
- malaise,
- abdominal pain,
- tachycardia,
- vaginal bleeding,
- foul-smelling bloody yellow discharge.
- uterus boggy and tender,
- rebound and cervical-motion tenderness are present
- the cervix may be open or closed.
Diagnosis
Ultrasound scan shows thickened endometrium or retained products of conception. The microorganisms responsible are most often Staphylococcus aureus, gram-negative bacilli, or gram-positive cocci, but the infection can be polymicrobial. Sepsis involving Clostridium sordellii has occurred after mifepristone-induced abortion.
Management
Evacuation of the uterus if products retained and IV antibiotics are required.
Hydatidiform Mole #
Hydatidiform mole, also known as a molar pregnancy or gestational trophoblastic disease,
- Incidence is 1 per 1,000 conceptions in the United States. Some parts of Asia have a rate that is significantly greater.
Complete molar pregnancy,
- a sperm fertilizes a defective egg without a nucleus and duplicates its own chromosomes
- there is no maternal genetic contribution and no embryo, only a malformed placenta that proliferates as rapidly growing, grapelike fluid-filled vesicles.
Partial molar pregnancy
- usually begins with a normal egg, which is either fertilized by two sperm or fertilized by one sperm followed by duplication of paternal chromosomes.
- The pregnancy can be triploid (69 XXX or 69 XXY instead of 46 XX or 46 XY) or even tetraploid, and can include fetal parts.
- An embryo begins to develop, but soon dies, and the abnormal placental tissue fills and distends the uterus as with a complete mole.
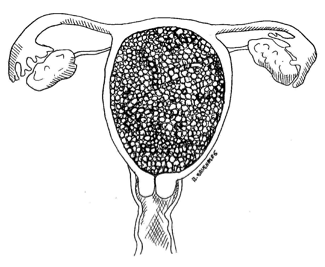
Signs and Symptoms
The pregnancy with hydatidiform mole includes the following signs:
- Uterus large for dates
- Absence of fetal heart
- Quantitative HCG levels much greater than expected
Women with a hydatidiform mole are more likely to experience:
- Hyperemesis gravidarum,
- Hyperthyroidism
- Preeclampsia <20 weeks
- vaginal bleeding – often the color of prune juice – but may be bright red.
Diagnosis is made by ultrasound.
Management
The mole is removed by surgical evacuation. Women with a history of molar pregnancy are at increased risk for choriocarcinoma, an aggressive cancer of the uterus so women are asked not to conceive for up to one year, and regular BHcG levels should be obtained.
Midwifery Management with Early Pregnancy Bleeding < 20 weeks
Always suspect ectopic pregnancy when a woman of childbearing age presents with lower abdominal pain or vaginal bleeding. This is true even if she denies that she could be pregnant, has not missed a period, or has undergone tubal ligation.
- Assess for hemodynamic instability or significant vaginal bleeding, take orthostatic vital signs, and perform abdominal and pelvic examinations.
- Initiate emergency fluid resuscitation in cases of orthostatic hypotension, and move fast. With early diagnosis, treatment is less invasive, and the likelihood of tubal rupture is reduced.
- Provide sensitive woman centered care including counseling, emotional and physical support.
Other causes of bleeding include friable cervix, polyps, infection, placenta previa, cervical or vaginal cancer and these can result in vaginal bleeding that usually presents with light, intermittent, and painless bleeding. Pregnancy loss is a more common occurance than an ectopic pregnancy. Cervical insufficiency usually presents with vague symptoms, which can include bleeding, change in vaginal discharge, pressure, and vague uncomfortable sensations.
Assessment should include:
- History
- Physical Exam
- Laboratory and Imaging investigations
Begin your assessment by taking a history.
Concurrently assess if she alert and animated, or distracted and withdrawn? Assess skin color, temperature, and moisture—pink and well perfused or pale and clammy? Triage accordingly – if acute – ABCs and seek higher level of care.
In obtaining history focus on:
Assess for risk factors:
- For spontaneous abortion: history of two or more consecutive pregnancy losses, bicornuate uterus, thrombophilic disorder
- For ectopic: history of smoking, tubal surgery/ disease, or assisted reproduction.
Examination:
- Take pulse and blood pressure supine, then standing
- a drop of >20 mmHg systolic or >10 mmHg diastolic along with tachycardia within 3 min of standing can be indicative of a significant bleed.
- Take Temp
- Gently percuss or palpate the woman’s abdomen for uterine size and pain, starting where she is feeling the least pain and examining the painful area last.
- Is her stated gestational age concordant with your physical assessment?
- Spontaneous abortion usually presents with midline pain
- Ectopic pregnancy typically involves unilateral pain that may radiate to the right shoulder.
- If febrile and uterus is tender suspect concomittent infection
- Auscultate FHR: a FHR may be more easily identified early in gestation during bimanual examination by lifting the uterus while the other hand holds the Doppler suprapubically.
- Examine the external genitalia and anus for any potential sites of bleeding.
- Speculum Exam:
- Inspect the vaginal vault, sidewalls, and cervix for signs of vaginitis, trauma, vaginal or cervical neoplasia, warts, or polyps.
- Take cultures
- Pelvic bimanual exam: This should be undertaken with great care. Gently palpate for adnexal mass, uterine enlargement or pain. A uterus enlarged by fibroids is irregularly shaped, while multiple pregnancy or hydatidiform mole causes uniform enlargement. If an ectopic pregnancy is present, the provider may palpate an adnexal mass or uterine enlargement or elicit pain with cervical motion or adnexal palpation; but often the examination reveals no unusual findings
Speculum Exam Findings
Dilation Closed or open? In parous women, external os may appear open, but internal os should be closed If inner os open or bleeding is heavy – suspect retained products of conception Membranes may be viewed through open cervix Bleeding A Friable cervix and cervical extropion common in pregnancy. Cervical bleeding from light touch is common. Use sponge sticks with gauze sponges on ring forceps to remove pooled blood/ clots. TissueRemove products of conception that may be wedged in the os with ring forcepts – send to pathology Examine any tissue passed. Probe blood clots for products of conception. The fetus will probably be passed whole, membranes appear as cellophane-like material, placental tissue has feathery chorionic villi more identifiable when floated in water. Usually, the products of conception are light-colored—tan or gray—and blood clots are dark red. Wesicles of a hydatidiform mole are grapelike, appearing like red currant jelly in prune juice.
- If the miscarriage is complete, the cervix may be either open or closed, the uterus will feel small and tightly contracted and bleeding and cramping will become minimal.
- If there is not incontrovertible evidence that all products of conception have passed, follow serial HCG levels until they become undetectable.
Other examinations that may be included:
- Culdocentesis: an 18- to 20-gauge needle is introduced through the posterior fornix and aspirating for fluid. Non-clotting frank blood in the cul-de-sac indicates ectopic pregnancy, while thin, pink fluid indicates a ruptured ovarian cyst.
- Uterine curettage may be done with low or abnormally rising beta-HCG levels, or those with levels above the discriminatory zone with no IUP visible on ultrasound. This procedure is performed to avoid unnecessary methotrexate treatment for women without ectopic pregnancy, but it carries the risk of disrupting a viable pregnancy. If HCG levels do not fall by 15% within 12 hr of D&C, ectopic pregnancy is likely (Tulandi, 2007a).
Laboratory and Imaging
- Obtain Serum BHcG for discriminate range and reassess at > 48 hour intervals when a Pregnancy of Unknown Location (PUL) is reported to assess level rise/ fall.
- Rh status – if unknown
- CBC may be indicated if bleeding excessive
- Vaginal and cervical cultures should be part of speculum exam
- Transvaginal Ultrasound should be ordered STAT to confirm intrauterine pregnancy and rule out ectopic.
Treatment / Consultation or Transfer of Care
- The urgency of the treatment will be guided by the woman’s status
- Assess maternal status and resuscitate / ABCs while seeking higher level of care
- If ectopic pregnancy is suspected or diagnosed inform the woman and arrange immediate referal to an obstetrician for methotrexate or surgical intervention.
- Incomplete or septic abortions usually require an Obstetrical consult / transfer for urgent management.
- Referral for medical or surgical management is also indicated for women who are stable with missed, incomplete abortions, or vaginal infections.
- Consult promptly for any cervical lesions
- Women who are Rh negative should recieve WinRho as soon as possible if the father of the baby cannot be confirmed to be Rh negative.
Antepartum Hemorrhage #
- Vaginal bleeding at any time after 20 weeks
- Affects 2 – 5% of pregnancies

Physiology #
- The non-gravid uterus is perfused by less than 1% of the woman’s circulating blood volume.
- In pregnancy the uterine blood flow increases to 20% of circulating blood volume, and by term 800mL of blood is circulated to the uterus every minute.
- Uterine bleeding during pregnancy and the postpartum can be catastrophic and lead to significant hemodynamic instability.
- Hemorrhage is a leading cause of maternal mortality worldwide.
Causes of APH #
- Abruptio
- Placenta Previa
- Lower genital tract lesions
- Vasa Previa
- Coagulopathy
- Unclassified
Abruptio #
The premature separation of the placenta from the uterine wall
Incidence: 0.5 – 1%
Pathophysiology #
- There is bleeding into the decidua basalis
- This bleeding can spread into the myometrium and the serosa > causing Couvelair uterus http://en.wikipedia.org/wiki/Couvelaire_uterus
- Bleeding may be trapped behind the placenta, leak through the cervix, or enter the amniotic compartment.
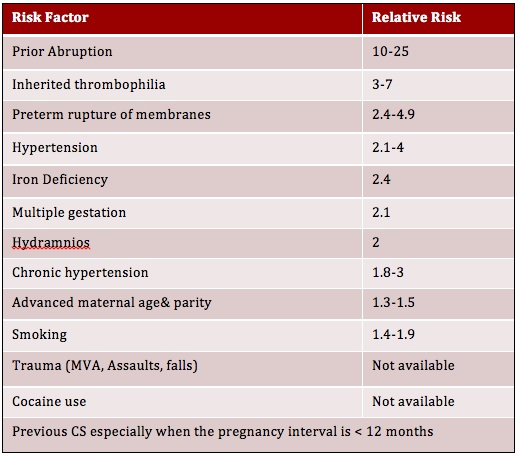
Most Abruptions are idiopathic
Diagnosis
- History and physical exam
- Defer vaginal exam pending ultrsound to rule out PREVIA
- Note: Ultrasound does NOT reliably diagnose an abruption, an organized clot can resemble the placenta
- Maternal vital signs
- Gentle speculum exam to examine the cervix for dilation and genital tract lesion
- EFM – to assess for signs of fetal compromise
o May find late decelerations with frequent low amplitude contraction pattern
- Tender, painful uterus
- Uterine Tone
o Frequent low amplitude contractions – “irritable uterus”
o Decreased resting tone – can be board like
o Uterine tachysystole
- Frank Bleeding
o May not have any visible blood loss if
- CONCEALED abruption
- Collecting behind placenta
- Contained in amniotic fluid
Placenta Previa #
- The placenta is implanted in the lower uterine segment and covers or partially covers the cervical os
- Incidence = 0.3-0.4 % of all birth
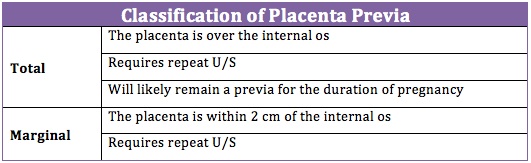
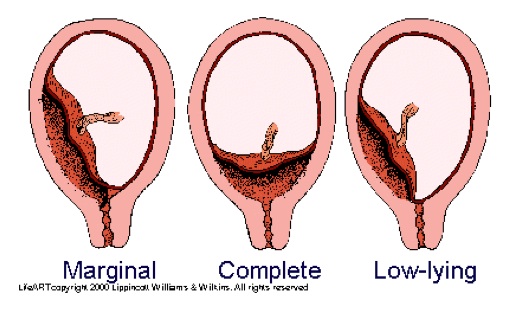
Note: the identification of a low lying placenta is NOT a placenta previa
o Here the leading edge of the placenta is 2-3 cm from the os
o This placement is not associated with an increased risk of hemorrhage and requires no additional follow up
Diagnosis #
Ultrasound #
o Locates placenta
o Measures distance from leading edge to os
Transabdominal US #
o Detects 85% of placenta previa in the 2nd trimester
o Has a false positive rate of 25%
o Has a false negative rate of 7%
Transvaginal US #
o Gold standard for diagnosis of placenta previa
o Sensitivity 87.5%
o Specificity 98.8%
o Positive predictive value 93.3%
o Negative predictive value 97.6%
Associated Factors #
- Previous Placenta Previa
- Previous C/S or uterine surgery
o Higher risk if interpregnancy interval is < 12 months
o Risk of accrete increases with # of prior C/S
- Advanced maternal age > 35 years
- Multiparity
- Smoking and Cocaine use in pregnancy
- Multiple gestation (succenturiate lobe increased)
Placenta Previa contributes to #
- Malpresentation
- Intrauterine growth restriction
- Placenta accreta
o Higher with prior C/S
- > 30% if 2 prior C/S
- > 50% if 3 prior C/S
- Antepartum hemorrhage
- Postpartum hemorrhage
Presentation #
- Painless antepartum bleeding
o Bright red or brown
o With soft non-tender uterus
o May have signs of fetal compromise
o May have signs of maternal compromise
- High presenting part
- Malpresentation
- Diagnosis on ultrasound
o Make clear on requisition you are ruling out placenta previa!
Management #
- Usually first diagnosed on 2nd trimester U/S
o At 17 weeks gestation 5-15% of pregnancies have placental tissue covering cervical os
o 90% of these cases are resolved by term
o Repeat U/S at 28-30 weeks gestation
o If still previa – repeat scan >35 weeks
- Expectant Management is appropriate in stable women
- 75% of women with placenta previa experience episodes of bleeding by 29 weeks gestation.
- 46% will delivery preterm, usually due to antepartum hemorrhage
- Recommend C/S at 37 weeks
o With adult ICU and blood products available
Vasa Previa #
Vasa Previa occurs when a fetal blood vessel runs through the membranes and travels over the cervical OS in front of the presenting part.
Incidence: 1 in 5000 births – the rate is higher in multiples due to an increase in succenturiate lobes
Vasa Previa is incompatible with vaginal birth. A C/S should be performed near term if diagnosed prior to labour.
Mortality is very high if the vessel ruptures.
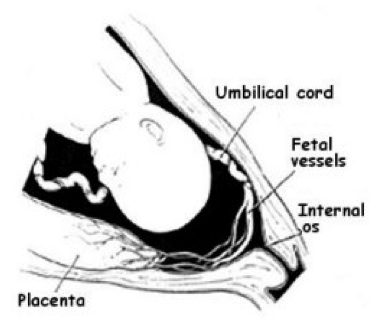
Associated Factors #
- Velamentous cord insertion
- In vitro fertilization
- Placenta Previa
- Succenturiate lobe
o Increased in low lying or placenta previa
o Vessels run through membranes over internal os
o Identifiable with colour doppler
Diagnosis #
- Ultrasound
- May palpate fetal vessel on VE with intact membranes
- Signs of fetal compromise with relatively small painless blood loss after ROM
o Total fetal blood volume approximately 80-100mL / kg
o Mortality is high if vessel ruptures as fetus can quickly exanguinate
- APT test for fetal hemoglobin may be performed
o 10mL of 0.1% NaOH
o Fetal sample will be pink. Maternal blood will be brown.
Management of Vasa Previa #
- If diagnosed in pregnancy – deliver near term by C/S
- If diagnosed in labour during Vaginal Exam
o REMOVE hand immediately
o Ask women to get into knee chest
o Call for help – alert EMS, Hospital, OR staff
o Prepare for emergency C/S
o Discontinue oxytocin
o Administer tocolytic
- If diagnosed after rupture
o Intrauterine resuscitation
o Emergency C/S
Clinical Tip #
Routinely palpate the membranes on VE and especially before performing an amniotomy. If a thin rope like structure is felt do NOT rupture membranes and assume a Vasa Previa until proven otherwise.
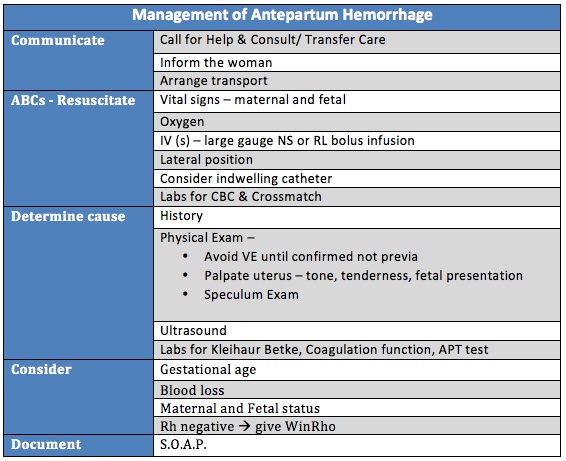
Management of Antepartum Hemorrhage #
If you receive a call / page from client: #
- Advise woman of urgency of situation
- Instruct her to lie down on her side.
- Instruct her to contact EMS or be taken directly to hospital
- Advise hospital maternity unit & OB of expected arrival time and her history
- Document
- Make it a practice to
o Ensure hospital has copy of antenatal record (at 20 and 36 weeks)
o Ensure hospital is copied Canadian Blood Services and Ultrasound reports
With History of bleeding: #
1. Assess in person- meet in hospital
2. Avoid VE until you can confirm placental location
a. Review 2nd trimester Ultrasound
3. Manage according to maternal status and fetal viability
a. Assess blood loss
b. Maternal Vital Signs
c. Fetal Heart rate (EFM if gestational age appropriate)
4. Conservative Management is appropriate if fetus is not term and both woman and fetus are stable.
5. Operative birth may be indicated pending status of woman and fetus.
6. Rhogam is indicated if woman is Rh negative
7. Document
Summary #
- Vaginal bleeding after 20 weeks is caused by:
- Abruptio
- Placenta Previa
- Vasa Previa
- Cervical lesions
- Coagulopathy
- Bleeding requires in person evaluation
- Vaginal exams must be avoided until confirmation of placental location
- Resuscitate by addressing ABCs, assess maternal status
- Determine cause of bleeding
- Evaluate the status of mother and fetus to inform further management.
