Anatomical and physiological considerations of labor: #
1- Uterus:
Uterus consists of two major but unequal parts: The body, and the cervix. The cervix is located between the external and internal os.The “isthmus” is that portion of the uterus between the internal cervical os and the endometrial cavity.
The uterus is composed of smooth muscles called myometrium whereas the cervix is composed of 90% collagen and elastic fibers and only 10% smooth muscle. The remarkable ability of cervix to dilate during labor is the result of dissociation of collagen by prostaglandins.
The transition between predominantly collagenous tissue of cervix to muscular tissue of the uterus is generally abrupt and occurs at the uterine isthmus.
During the first 36 to 38 weeks of pregnancy the myometrium is unresponsive. Near the end of pregnancy the increase in the myometrial activity and contractibility results in Braxton Hicks contractions. These contractions prepare the uterus by stretching the uterine isthmus which is gradually converted to the lower uterine segment. The lower segment is the passive roomy part that accommodates the fetal head.
Braxton Hicks contractions may be quite painful and must be distinguished from those of true labor. Braxton Hicks contractions are irregular, short, and brief and do not change the dilatation of effacement of the cervix. Whereas contractions of true labor are not only painful but they gradually become more regular, stronger, and last longer. The most important predictor of true labor is change in cervical dilatation and/or effacement.
With the onset of active labor the uterus transforms into two distinct parts. The upper uterine segment or fundus contracts actively and pushes the presenting part into the passive lower uterine segment which at this stage is greatly expanded and thinned-out.
The unique arrangement of myometrial smooth muscles facilitates greater shortening and force-generating capacity compared to other smooth muscles. This is required to effectively push the baby into the birth canal during labor.
The myometrium of the upper segment does not relax to its original length after contractions rather it becomes relatively fixed at a shorter length. This results in effective expulsion of the fetus during labor.
The upper segment becomes progressively thickened during the first and second stages of labor and tremendously thickened immediately after delivery of the fetus.
2- Fetal head:
The fetal head at term is made up of two frontal, two parietal, two temporal, and one occipital bone. These bones are not united rigidly, but rather are separated/connected by membranous spaces called sutures. This allows considerable shifting or sliding of each bone to accommodate the size and shape of maternal pelvis. This intrapartum process is called molding.
- Frontal suture is located between two frontal bones.
- Sagittal suture: Between two parietal bones
- Two Coronal sutures: Between frontal and parietal bones
- Two Lambdoid sutures: Between parietal and occipital bones
- Two temporal sutures: between parietal and temporal bones
Where several sutures meet an irregular space forms called fontanel. The two clinically important fontanels are anterior and posterior fontanels.
The anterior fontanel is a lozenge shaped space at the junction of sagittal and coronal sutures.
The posterior fontanel is a small triangular area at the junction of sagittal and coronal sutures.
The localization o these fontanels gives important information concerning the presentation and position of the fetus.
The biparietal diameter of the head extends from one partial bone to the other and is the greatest transverse diameter of the head. Page 135
3-Boney pelvis:
The pelvis is composed of four bones: Sacrum, Coccyx, and two innominate bones. Each innominate bone is formed by the fusion of ilium, ischium, and pubis. The innominate bones are joined to the sacrum at the sacroiliac joint and to one another at the symphysis pubis.
The ischial spines are in mid pelvis and are halfway between the pelvic inlet and the pelvic outlet. Ischial spines are of great obstetrical importance. They can be ready palpated on the pelvic side wall during vaginal exam and serve as valuable landmarks in assessing the level to which against which the presenting part of the fetus is descended into the true pelvis.
The pelvic inlet has four diameters and is rather round in gynecoid pelvis. The antero-posterior, transverse and two obliques. Use a Figure here. A normal sized head usually enters the pelvic inlet in the transverse or one of the oblique diameters.
The distance between two ischial spines is the shortest diameter of the pelvic cavity.
We should briefly mention different pelvis types. No need to go into details of non gynecoid pelves.
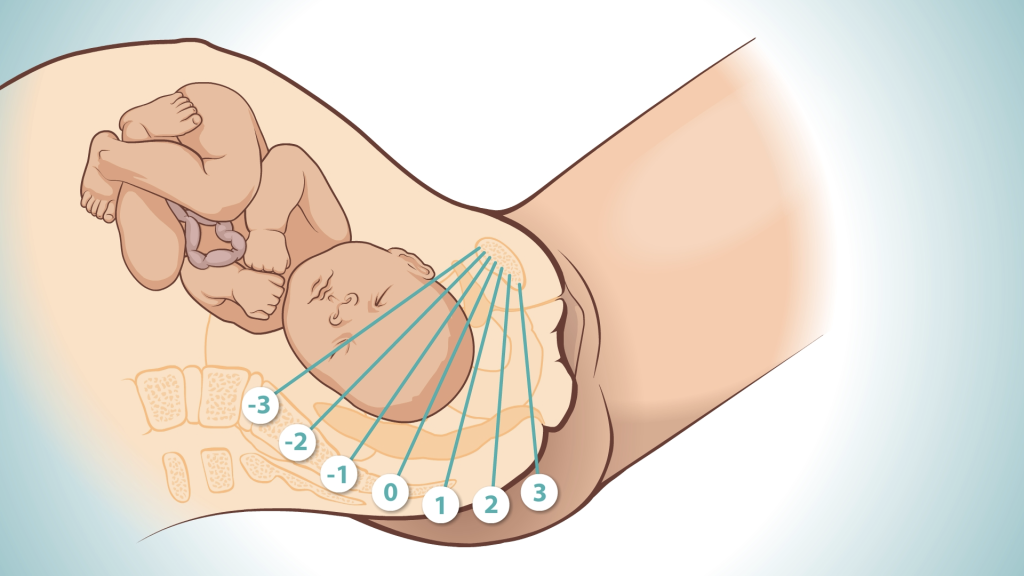
4- Fetal station:
When the biparietal diameter of the normally flexed fetal head has passed through the pelvic inlet, the head is engaged. At this time the lowermost portion of the head is at the level of the ischial spines, it is designated as being at zero (0) station. The pelvis above and below the spines is divided into fifths. Thus as the presenting fetal part descends from the inlet toward the ischial spines the designation is -5, -4, -3, -2, -1, then 0 station. Below the ischial spines the presenting fetal part passes +1, +2, +3, +4, and +5 stations to delivery. Station +5 corresponds to the fetal head being visible at the introitus.
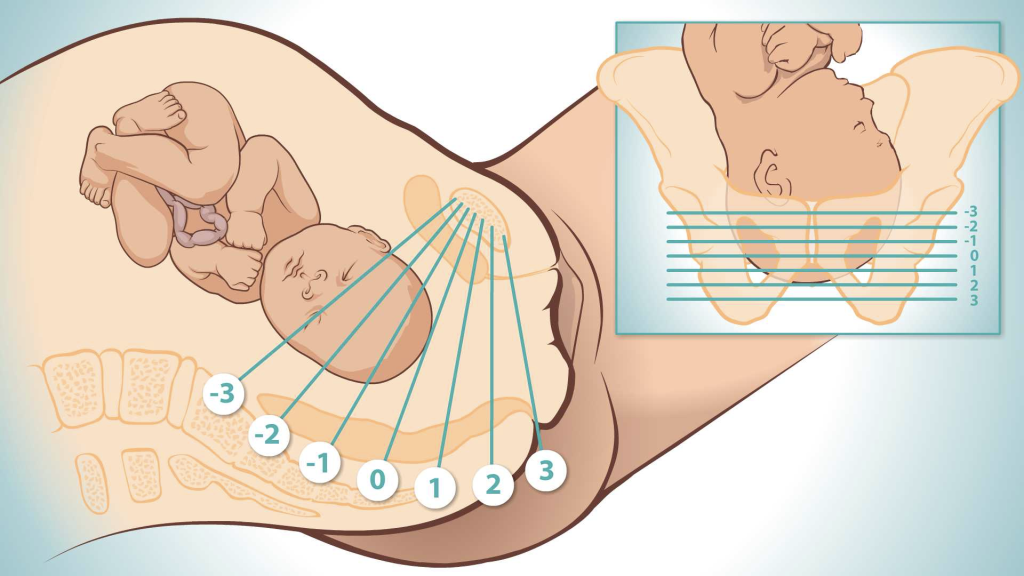
The distance from the plane of pelvic inlet to the level of ischial spines is approximately 5 cm in most pelves and the distance from the biparietal plane of the fetal head to the vertex is about 3-4 cm. Under these circumstances the vertex cannot possibly reach the level of spines unless the biparietal has passed the inlet.
If the head is unusually molded, or if there is an extensive caput or both, the engagement might not have taken place even though the head appears to be at 0 station.
5- Fetal position:
Refers to the relation of an arbitrarily chosen portion the fetal head to the right or left side of the maternal birth canal. The fetal occiput (posterior fontanel) is the determining point in cephalic presentation. The posterior fontanel is triangular and smaller than the anterior fontanels which is diamond shaped. These two fontanels can be distinguished by palpation during vaginal exam during labor.
For more accurate orientation the relation of occiput to the anterior, transverse, or posterior portion of maternal pelvis is considered. There are six possible positions depending on where the occiput lies in relation to the maternal pelvis.
Explain the ROA, ROT, ROP and then LOA, LOT, LOP here.
During vaginal examination the fingers are introduced into the posterior aspect of the vagina. The fingers are then swept forward over the fetal head toward the symphysis. Fig 12-11 During this movement the fingers necessarily cross the fetal sagittal suture. When it is felt, its course is outlined, with small and large fontanels at the opposite ends. These two fontanels are then carefully examined and differentiated based on their shape and size.
Stages of labor:
I. First stage – onset of labor to complete dilatation
- Latent phase
- Active phase
II. Second stage
III. Third stage
1st stage of labor begins with active uterine contractions that bring about effacement and dilatation of the cervix. The cervix, which was softened during the phase of uterine preparation, becomes shorter and dilates. These are called effacement and dilatation.
“Show” is discharge of small amount of blood-tinged mucus from the vagina provided rectal or vaginal examinations have not been performed in the preceding 48 hrs. This represents the expulsion of the mucus plug that had filled the cervical canal during pregnancy. It is a rather dependable sign of impending onset of labor.
The first stage ends when the cervix is 10 cm or fully dilated and has two phases: latent phase (up to 4 cm dilatation) and active phase (from 6-10 cm).
The Seven Cardinal Movements
Over the course of delivery, the fetus moves through seven positions, known as the 7 Cardinal Movements, which assist the baby in the passage through the birth canal.
In a normal vertex presentation, most fetuses initiate the cardinal movements in an occiput transverse or oblique position.
The first Cardinal Movement is called Engagement, and occurs when the biparietal diameter of the fetal head has entered the pelvic inlet, and the vertex is at the level of the ischial spines. As the labour continues, the head moves down into the pelvis. This is called Descent. Descent often occurs quickly after Engagement, and may occur before the cervix is fully dilated and effaced.As soon as the descending head meets resistance, whether from the cervix, walls of the pelvis, or pelvic floor, flexion of the head normally results. The chin is brought into more intimate contact with the fetal thorax and the larger occipto frontal diameter of the head is substituted with the smaller suboccipito bragmatic diameter which facilitates the descent.
#
Engagment #

Descent #
Due to the anatomy of the pelvis, the fetal head is forced to rotate from a transverse position to an occiput anterior position, with the occiput against the symphysis pubis and the face toward the mother’s back. This movement, known as Internal Rotation, allows the fetal head to pass through the widest opening of the pelvic outlet.
As the head passes under the mother’s pubic bone and begins to crown, it undergoes extension. Because the vulvar outlet is directed upward and forward extension must occur before the head can pass through it. With progressive distention of the perineum and vaginal opening an increasingly larger portion of the occiput gradually appears. The head is born by further extension as the o
cciput, forehead, nose, mouth, and finally the chin pass successively over the perineum. Immediately after its birth, the head drops downward so that the chin lies over the maternal anal region. If a nuchal cord is present it could be slipped over the head before delivery of the shoulders.
The delivered head next undergoes restitution or external rotation. The head rotates back to the oblique and then transverse position. This movement corresponds to the rotation of the fetal body serving to bring the shoulders into relation with the antero-posterior diameter of the pelvic outlet. Thus one shoulder is anterior, behind the symphysis, and the other is posterior.
Almost immediately after external rotation the anterior shoulder appears under the symphysis and the perineum soon becomes distended by the posterior shoulder. This is the beginning of the final movement, called Expulsion. After delivery of the shoulders the rest of the body is quickly extruded.
Third Stage of Delivery:
