Learning Objectives #
Upon completion of this chapter, you should be able to:
- Identify babies who require respiratory support or interventions.
- Apply the Respiratory Sequence.
- Determine oxygen requirements and select an appropriate oxygen delivery method.
- Use the Respiratory Score to organize care on the basis of the severity of respiratory distress.
- Recognize the need for and how to initiate respiratory support.
- Perform basic interpretation of chest radiographs and blood gas results.
- Recognize and manage the common causes of respiratory distress.
- Recognize when to exit to the other ACoRN Sequences.
Key Concepts #
- Establishment of ventilation and prevention of hypoxia are required for successful transition from fetal to neonatal circulation.
- Oxygenation is critical for cellular, tissue, and organ function.
- The most common cause of cardiorespiratory failure in the newborn is hypoxemia; this is corrected by adequate ventilation and oxygenation.
- Processes that interfere with the inflation and subsequent ventilation of the newborn lungs cause respiratory distress.
- The goal of early detection and intervention for respiratory distress is to optimize ventilation and oxygenation.
- Severe respiratory distress is a precursor of respiratory failure.
- Babies with severe respiratory distress, or frequent or intermittent apnea or gasping respirations require immediate attention including intubation and ventilation.
- Respiratory distress may be a sign of infection requiring immediate treatment.
- Preterm babies have poor respiratory reserve and may require earlier intervention.
- The ACoRN Respiratory Score provides guidance for intervention.
- Babies with increasing oxygen requirements require close observation.
Skills
- Blood gas interpretation
- Chest radiograph interpretation
- Continuous positive airway pressure (CPAP)
- Emergency vascular access – Umbilical vein catheterization
- End-tidal CO2 detector
- Free flow oxygen administration
- Mechanical ventilation
- Pneumothorax – Chest transillumination
- Pneumothorax – Chest tube insertion
- Pneumothorax – Needle aspiration
- Premedication for intubation
- Pulse oximetry
- Surfactant
Introduction #
The Respiratory Sequence is the first area of concern in the ACoRN Primary Survey, reflecting the critical importance of establishing and maintaining adequate ventilation and oxygenation in the management of the unwell and at-risk newborn.
Transient or ongoing respiratory disorders are among the most common conditions encountered in neonatal care, particularly in preterm babies. Attention to the early signs and symptoms of respiratory insufficiency will often prevent later deterioration or instability.
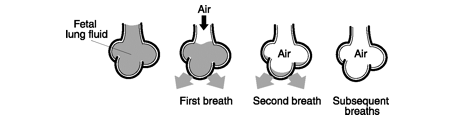
Successful cardiopulmonary transition from intrauterine to extrauterine life involves a series of changes, starting with the aeration, and ventilation of the lungs immediately after birth.
 #
#
During this process, fluid in the alveoli is replaced by air, and blood flow to the lung increases as the pulmonary blood vessels dilate.
At the same time, with the clamping of the umbilical cord, systemic vascular resistance rises and exceeds pulmonary vascular resistance, resulting in the closure of the foramen ovale. Gas exchange at the alveolar level increases the oxygen level in the blood, further decreasing the pulmonary vascular resistance, and eliminates carbon dioxide. The ductus arteriosus constricts, and the normal newborn ventilation and circulation are established.
A delay or inability to complete the normal transition to extrauterine life results in neonatal respiratory problems, such as when,
- reabsorption of alveolar fluid is delayed: transient tachypnea of the newborn
- alveoli do not stay inflated after the alveolar fluid is reabsorbed due to surfactant deficiency: respiratory distress syndrome
- small airways and alveoli become obstructed: aspiration syndromes
- lungs become infected: pneumonia
- pulmonary pressure remains high: persistent pulmonary hypertension of the newborn
- lungs suffer external compression: pneumothorax
- lungs are hypoplastic: congenital diaphragmatic hernia or prolonged severe oligohydramnios starting in the second trimester.
Respiratory Sequence #
Alerting Signs #
A baby who demonstrates one or more of the following Alerting Signs enters the Respiratory Sequence:
Laboured respiration #
A baby with laboured respiration is also described as having respiratory distress, difficulty breathing, or increased work of breathing. The signs of laboured respiration are:
- nasal flaring – outward flaring movements of the nostrils on inspiration in an attempt to move more air into the lungs.
- grunting – audible sounds produced as the baby exhales against a partially closed glottis in an effort to maintain end-expiratory pressure.
- intercostal indrawing – retractions of the intercostal spaces due to increased negative pressure within the chest.
- sternal retractions – paradoxical backward movements of the sternum on inspiration due to increased negative pressure within the chest.
- gasping – an ominous sign of cerebral hypoxia characterized by deep, single or stacked, slow and irregular, terminal breaths.
Respiratory rate #
The normal newborn respiratory rate is 40 to 60/minute. A respiratory rate > 60/minute (tachypnea) usually indicates respiratory difficulty or distress.
Receiving respiratory #
This Alerting Sign identifies babies who are receiving ongoing respiratory support, with continuous positive pressure ventilation (CPAP) or positive pressure ventilation (manual or mechanical). Because the respiratory insufficiency is ongoing, these babies require further evaluation and management.
Core Steps #
Core steps are the interventions and monitoring activities applicable to all babies entering the Respiratory Sequence. These include,
- recheck patent airway/breathing
- administer O2 as needed to maintain SpO2 88 to 95%
- establish/continue monitors: pulse oximetry, cardiorespiratory, blood pressure, oxygen analyzer
- calculate the Respiratory Score in spontaneously breathing babies.
Respiratory Score #
Judging the severity of respiratory distress is a skill acquired with experience. The Respiratory Score assists the clinician to recognize the components that need assessment. The Score is utilized in babies who are breathing spontaneously, including those being treated with CPAP. It is not utilized in babies who are receiving ventilation assistance.
The Table lists the 6 components of respiratory assessment and their descriptors. The first 5 components help quantify the degree of respiratory distress. The degree of prematurity has been included in the score as it is the main modifier of the baby’s ability to cope with a given degree of respiratory distress.
Each component is scored from 0 to 2.
The Respiratory Score is the sum of the 6 individual scores.
The Respiratory Score is also useful for tracking the severity of respiratory distress over time in a baby who is breathing spontaneously.
The interpretation of the Respiratory Score and its use by itself or in conjunction with other findings is described under Organization of Care.
Organization of Care #
The objectives in the care of babies with respiratory problems are to ensure that ventilation and oxygenation are adequate, and to provide early intervention and support as required.
The organization of care is based primarily on the severity of respiratory distress as identified using the Respiratory Score, and secondarily on additional clinical information.
Mild respiratory distress
- Respiratory Score < 5, starting at birth and lasting < 4 hours.
Moderate respiratory distress
- Respiratory Score of 5 to 8
- mild respiratory distress (Respiratory Score < 5), but persisting over 4 hours
- babies who were previously well but develop new respiratory distress.
These babies are at risk of progressing to respiratory failure. Babies with persistent or new respiratory distress may be symptomatic due to other causes such as infection.
Severe respiratory distress
- Respiratory Score > 8
- babies with severe apnea or gasping
- babies who are already receiving ventilation due to respiratory failure diagnosed during the Resuscitation Sequence or a previous passage through the Respiratory Sequence.
Other factors that increase the risk a baby will be unable to sustain breathing (respiratory failure) include,
- the degree of prematurity
1.babies whose gestational age is < 27 weeks usually require respiratory support
2.babies whose gestational age is < 30 weeks and/or birth weight < 1500 grams are at increased risk of requiring respiratory support
- oxygen requirements > 50%, which indicate that the baby has little reserve.
Response #
Babies with mild respiratory distress lasting less than four hours require,
- ongoing observation
- oxygen supplementation to maintain blood oxygen levels in the desired range (such as, SpO2 between 88 to 95%)
- further work-up if they meet criteria for entry into the Infection Sequence.
Babies with moderate respiratory distress may need some degree of respiratory support, such as CPAP or, sometimes, mechanical ventilation to prevent progression to severe respiratory distress and respiratory failure.
Babies with severe respiratory distress, including severe apnea or gasping, require immediate attention including intubation and ventilation, as these are ominous signs of respiratory failure.
Once initiated, ventilation needs to be optimized to,
- decrease the work of breathing
- maintain the SpO2 in the desired range, such as between 88 to 95%
- restore acid base balance (pH between 7.25 and 7.40)
- maintain PCO2 between 45 and 55.
Babies receiving respiratory support (CPAP or ventilation) require,
- vascular access to initiate D10%W solution
- chest radiograph
- blood gases
- consideration for immediate consult, depending on expertise and resources.
Continuous positive airway pressure (CPAP)
Mechanical ventilation
Next Steps #
The Next Steps are to obtain a focused history, conduct a physical examination, order diagnostic tests and establish a working diagnosis.
Focused respiratory history #
Important information to gather during the focused respiratory history includes:
Antepartum
- gestation and accuracy of dates
- antenatal ultrasound findings
- maternal diabetes
- maternal Group B streptococcus (GBS) status (positive, negative, unknown)
- administration of antenatal steroids
- maternal substance use
- family history of neonatal respiratory disorders
Intrapartum
- presence of non-reassuring fetal health surveillance during labour and delivery
- presence of meconium stained liquor
- duration of rupture of membranes
- evidence of chorioamnionitis (maternal fever and/or fetal tachycardia)
- nature of labour and route of delivery
- medications
- administration of intrapartum antibiotics for GBS prophylaxis
Neonatal
- results of umbilical cord blood gas (arterial and venous) determination, if done
- condition at birth, including Apgar score
- resuscitation efforts required and response
- time of onset of symptoms, i.e., present from birth or developed after a period of normal respiratory function
- gestational age and birth weight
Physical examination #
The essential components of the physical examination include:
Observation
- work of breathing and symmetry of chest movement
- indicators of laboured respiration (nasal flaring, intercostal indrawing, sternal retraction, and gasping)
- skin colour and mucous membranes for evidence of central cyanosis
- respiratory support (for example, size and position of endotracheal tube, ventilator settings, and inspired oxygen)
Measurement of vital signs: respiratory rate, heart rate, temperature, blood pressure, and oxygen saturation.
Examination
- auscultate both lung fields laterally for equality and nature of breath sounds. Diminished breath sounds unilaterally may signal intubation of the right bronchus, pneumonia, an area of atelectasis, or presence of a pneumothorax or other space-occupying lesion (for example, a diaphragmatic hernia).
- presence of grunting, inspiratory stridor, audible expiratory wheeze, crackles)
- presence of cleft palate or micrognathia (small jaw)
Diagnostic #
Diagnostic tests are performed on all babies entering the Respiratory Sequence. The exception is a term baby with mild respiratory distress lasting less than four hours.
Two diagnostic tests that can assist in quickly reaching a working diagnosis for respiratory conditions are:
1. Chest radiograph
- To determine the cause of respiratory distress and guide intervention.
2.Blood gases
- Arterial, capillary and venous blood gases are used to assess the adequacy of ventilation (PCO2) and the presence of acidosis (pH and base deficit)
- Arterial blood gases are used to assess the adequacy of oxygenation (PO2)
Blood gases should be used in conjunction with pulse oximetry which provides a continuous assessment of oxygenation.
Establish a Working Diagnosis #
Formulation of a working diagnosis relies heavily on knowledge of the more common conditions that present as respiratory distress in the newborn, and their radiographic findings. These include,
- transient tachypnea of the newborn
- respiratory distress syndrome
- meconium aspiration syndrome
- pneumothorax and other air leaks
- pneumonia
Transient Tachypnea #
- Lung fluid production does not cease prior to birth and there is a delay in clearance of residual lung fluid after birth.
- Occurs as a primary cause of respiratory distress in term or near-term babies, and is more common in newborns born by cesarean section, especially when there has been no labor.
- Babies present with mild to moderate respiratory distress, with oxygen requirements usually < 40%.
- Respiratory distress due to transient tachypnea of the newborn will often resolve over the first few minutes to hours after birth as residual lung fluid is reabsorbed.
Respiratory Distress Syndrome #
- Lack of surfactant production/release in the lungs, resulting in progressive collapse of the terminal bronchioles/alveoli.
- Primarily a disease of preterm babies; its incidence increases with decreasing gestational age.
- Babies present with any degree of respiratory distress and oxygen requirements.
- Respiratory distress will worsen if respiratory effort or support is unable to prevent progressive lung collapse. When RDS is not treated with exogenous surfactant it will generally improve after 72 hours. During this time,
- endogenous surfactant production and release are established.
Meconium Aspiration Syndrome #
- Perinatal aspiration of meconium resulting in a combination of large and small airway obstruction, pneumonitis, surfactant inactivation, and ventilation:perfusion mismatch.
- A disease of post-term, term and, sometimes, near-term babies (with a functionally mature gastrointestinal tract) who are born in the presence of meconium. More common if the baby is depressed at birth or if meconium is thick or particulate.
- Babies may present with any degree of respiratory distress and oxygen requirements.
- May be accompanied by persistent pulmonary hypertension of the newborn.
- Severe MAS is life threatening and requires prompt specialized care.
Pneumothorax #
- Air leak within the pleural space.
- Primarily occurs in babies with lung disease (aspiration syndromes and RDS) receiving respiratory support (CPAP or ventilation). May also occur with spontaneous respirations and in the absence of lung disease (during initial spontaneous breaths).
- Babies present with an acute increase in respiratory distress and oxygen requirements.
- Tension pneumothorax may present with sudden onset of cardiovascular collapse.
- A small pneumothorax is often minimally symptomatic.
- A moderate or large pneumothorax requires drainage via chest tube.
- A smaller pneumothorax with minimal respiratory distress (tachypnea only) and no cardiovascular deterioration can be observed until it resolves spontaneously.
Other radiographic signs found in air leaks:
- In pneumomediastinum, the thymus is outlined and may appear lifted from the cardiac surface giving the impression of a “butterfly” or “sail”.
- In pneumopericardium, a halo is seen around the heart.
Pneumonia #
- Infectious infiltrate of the lungs, usually interstitial and diffuse rather than lobar in appearance.
- It is more likely to occur in the presence of risk factors for sepsis (for example, prolonged rupture of membranes, maternal colonization with GBS, or chorioamnionitis).
- Babies may or may not be systemically ill at onset, but the clinical course may be fulminant.
- The inability to rule out pneumonia by clinical or radiographic appearance gives rise to the recommendation to treat all respiratory disease in the newborn with intravenous antibiotics.
Other causes of newborn respiratory insufficiency #
1. Persistent Pulmonary Hypertension of the Newborn (PPHN)
- Failure of the normal drop in pulmonary vascular resistance after birth, resulting in decreased pulmonary blood flow and in bi-directional or right-to-left shunting of blood through the ductus arteriosus or foramen ovale, and tricuspid regurgitation.
- Usually has an underlying vascular component of prenatal origin, which includes increased vascular muscularization and reactivity, decreased pulmonary vascularization, and/or abnormal vascular distribution.
- PPHN is usually triggered by respiratory conditions such as RDS, MAS, pneumonia, or congenital diaphragmatic hernia, but may also occur as a primary disturbance of transition in the absence of parenchymal lung disease.
- Presents with hypoxic respiratory failure (high oxygen requirements), labile oxygenation, and frequently with higher preductal than post ductal oxygenation as demonstrated by blood gas analysis or pulse oximetry. The diagnosis should always be confirmed by cardiology consultation and echocardiography to rule out abnormal cardiovascular anatomy.
- PPHN is life threatening and requires prompt specialized care.
2. Lung hypoplasia
- Overall decrease in the number of airways and gas-exchange spaces (alveolar sacs, or alveoli).
- Occurs in babies who experienced insufficient lung inflation in-utero due to:
- o severe oligohydramnios as a result of
- − rupture of the membranes in the second trimester
- − renal agenesis
- – urinary outflow obstruction.
- o congenital diaphragmatic hernia (CDH)
- o neuromuscular disease with decreased fetal respiration
- Presents at birth as profound respiratory distress.
- There is increased risk of PPHN and pneumothorax.
- Lung hypoplasia is life threatening and requires prompt specialized care.
Radiographic findings:
- Small lung fields, often with clear lung fields.
- In congenital diaphragmatic hernia, a space-occupying lesion is seen which is more commonly found on the left side.
Specific Management
Specific Management depends on the working diagnoses, and is discussed in the illustrative cases that follow.
Respiratory Cases #
In this section you will find a number of example cases, including ‘Mild respiratory distress in a term newborn’ and so on.
Respiratory Case # 1 – Mild respiratory distress in a term newborn #
A baby girl is born by Cesarean section at 38 weeks gestation. This was a planned elective section in view of a breech presentation. She was vigorous at birth. You are called to assess her in the recovery room at 30 minutes of age because the baby is grunting.
You find her to be dusky in room air, with regular respirations, mild nasal flaring, and audible grunting with stimulation. She has intercostal indrawing and mild sternal retractions. Her heart rate is 120 bpm.
What is duskiness?
Duskiness is a common term often used to describe central cyanosis.
Although her breathing is laboured, it is effective as the heart rate is > 100 bpm and respiration is regular, however, cyanosis is one of the Alerting Signs for immediate resuscitation.
You take the baby across the hall to the radiant warmer in the newborn resuscitation area.
You perform the Core Steps of the Resuscitation Sequence, and provide free flow oxygen by mask.
The baby’s breathing remains laboured but regular, respiratory rate is 70/minute, and heart rate 140 bpm. You note the baby’s color has improved in response to oxygen administration.
You exit the Resuscitation Sequence and complete the ACoRN Primary Survey.
Additional observations made in order to complete the ACoRN Primary Survey indicate that the baby is at risk for hypoglycemia because she is exhibiting respiratory distress and has not been fed, and the blood glucose is not known. The baby’s temperature is also unknown and she is at risk for temperature instability.
The baby exhibits two of the Alerting Signs for the Respiratory Sequence.
You enter the Respiratory Sequence and perform the Core Steps.
- place the flow inflating bag, oxygen mask or oxygen tubing close to the baby’s face
- use blended air/oxygen, or oxygen at a flow rate of 5 L/minute
- flow inflating bags allow delivery of the oxygen concentration desired, according to the setting on the blender
- oxygen masks and oxygen tubing do not allow delivery of the oxygen concentration desired, according to the setting on a blender, as room air is entrained to a variable degree; when attached to 100% oxygen
- oxygen masks deliver up to 50% oxygen
- oxygen tubing delivers up to 30% oxygen
Free-flow oxygen administration during resuscitation #
Oxygen administration to a spontaneously breathing baby during stabilization
Oxygen Hood:
- is placed over the baby’s head to contain the baby’s breathing environment
- blended humidified oxygen/air is administered at the desired concentration
- a gas flow 5 to 10 L/minute into the hood prevents CO2 accumulation
- able to administer desired oxygen concentration, according to the setting on the blender
- the exact amount of oxygen delivered can be determined using an oxygen analyzer placed close to the baby’s mouth
- oxygen concentration is adjusted by changing the setting on the blender to achieve the desired SpO2, such as between 88 to 95%
- the initial temperature
Incubator:
- incubators manufactured after 1990 are able to consistently administer high oxygen concentration, humidity and warmth, and have built-in oxygen analyzers that continuously adjust the oxygen flow to maintain a preset concentration
- older incubators may provide as little as 30% oxygen despite being flooded with 100% oxygen and are not able to maintain the oxygen concentration when the port-hole or door is opened
- o reliable oxygen administration requires simultaneous use of an oxygen hood when using older incubators.
Nasal prongs (newborn size):
- 100% oxygen is administered at a flow < 2 L/minute. Higher flows,
- o can cause inadvertent positive end expiratory pressure (PEEP)
- o irritate and dry the nasal mucosa
- oxygen flow is adjusted up or down to achieve the desired SpO2, such as between 88 to 95%
- not a preferred method of oxygen delivery during initial management because,
- o of the inability to determine the precise amount of oxygen the baby is receiving,
- o oxygen administered in this way is easily diluted by entrained air during crying, mouth breathing, or increased respiratory rate and depth of respiration.
Why is it important to measure the oxygen concentration delivered using an oxygen analyzer?
- to know if the baby’s oxygen requirements are increasing or decreasing over time, as oxygen requirements > 40 to 50% indicate there is a risk that the baby will not be able to sustain breathing or oxygenation
What measurements determine the amount of oxygen in the baby’s circulation?
- hemoglobin oxygen saturation (SO2)
- o pulse oximetry (SpO2)
- o arterial sample (SaO2)
- partial pressure of oxygen (PO2)
- o arterial sample (PaO2)
It is important to understand the difference between hemoglobin oxygen saturation (SO2) and the partial pressure of oxygen (PO2)
Oxygen is carried by the blood either bound to hemoglobin molecules, or dissolved in plasma in an approximate ratio of 40 to 1.
- SO2, measured in %, represents hemoglobin saturation, the percentage of hemoglobin molecules that are bound to oxygen.
- PO2, measured in mmHg, is the partial pressure exerted by the oxygen molecules dissolved in the plasma; the higher the PO2, the more oxygen binds to hemoglobin.
- o as PO2 drops in the capillary circulation, oxygen is released to the tissues
- o when PO2 increases in the alveolar capillaries oxygen binds to hemoglobin.
For practical purposes it is correct to assume that,
- SO2 determines how much oxygen is carried in the blood
- the maximum oxygen carrying capacity of the blood is reached once SO2 reaches 100%.
The relationship between PO2 and SO2 is figuratively expressed as the oxyhemoglobin dissociation curve.
- On the steep portion of the oxyhemoglobin dissociation curve, SO2 increases rapidly with PO2 until SO2 reaches approximately 75% and PO2 approximately 35 to 40 mmHg.
- On the flat portion of the curve, once SO2 exceeds 95%, large changes in PO2 result in small changes in SO2.
- o SO2 of 98 to 100% may reflect any value of PO2 ≥ 90 mmHg.
SaO2: Indicates how much oxygen is bound to hemoglobin in arterial blood. The amount of oxygen carried by the blood is proportional to the SaO2 and hemoglobin concentration, and not to the PaO2.
- the target range of SaO2 in newborns receiving oxygen is 88 to 95%
- SaO2 is a sensitive indicator of hypoxemia
- SaO2 is a poor indicator of hyperoxemia
- o once the PO2 is > 80 to 90 mmHg, SO2 will be 100% regardless of the PO2 value
- minimal additional oxygen is carried by blood with SaO2 > 95%.
PaO2: Indicates how well the lung is transferring inspired oxygen to the blood. The magnitude of impairment in lung function is proportional to the difference between inspired oxygen (%) and arterial oxygen (PaO2).
- the target range of PaO2 in a newborn is 50 to 70 mmHg
- hypoxemia (PaO2 < 50 mmHg) decreases blood flow to the lungs by increasing pulmonary vascular resistance
- yperoxemia (PaO2 > 70 to 90 mmHg) increases the risk of oxygen associated retinal injury in preterm infants (retinopathy of prematurity).
The ideal oxygen saturation range for babies is controversial, but values between 88 to 95% are generally recommended. Oxygen saturation values > 95% may be associated with high levels of blood oxygen which are potentially damaging to immature tissues, such as the retina of premature babies.
In the presence of good cardiac function, oxygen saturation in the normal range indirectly indicates adequate oxygen delivery to the tissues, and prevents the development of acidosis and pulmonary vasoconstriction.
Oxygen saturation monitoring provides a good indication of the effectiveness of respiratory interventions in oxygenating the blood, but is not an indicator of effective breathing or ventilation.
Pulse oximetry (SpO2) : Pulse oximetry is used frequently to monitor a baby’s oxygenation because it is non-invasive, easy to use, and provides immediate readings in a continuous display. SpO2 closely reflects SaO2.
Pulse oximetry #
You change the mode of oxygen administration to an oxygen hood, and determine the oxygen % required to maintain the SpO2 in the 88 to 95% range.
You calculate the Respiratory Score, assigning 1 point for each component: respiratory rate (60 to 80/minute), baby is receiving oxygen, mild retractions, and grunting only when disturbed. The baby’s gestational age is 38 weeks so you assign 0 points for prematurity.
You organize care on the basis of the Respiratory Score.
The baby has mild respiratory distress, with a respiratory score of 4 and no apnea.
She requires observation and continued monitoring.
The Focused history reveals that the mother’s pregnancy and cesarean section delivery were uneventful, and that there are no risk factors for infection: there was no maternal fever, membranes were ruptured at birth, and group B streptococcus screening was negative.
On Physical examination you note that she is pink on 30% oxygen and that SpO2 is 92%. The baby looks well despite her respiratory symptoms.
The clinical evaluation of a baby’s response to administration of oxygen includes the assessment of color and oxygenation, and effect on breathing.
You make a tentative diagnosis of transient tachypnea of the newborn and return to the ACoRN Problem List in order to address the Fluid & Glucose Management and Thermoregulation Sequences.
Mild respiratory distress due to transient tachypnea of the newborn will often resolve over the first few minutes to hours after birth as residual lung fluid is reabsorbed. Babies will require further assessment to confirm the diagnosis and guide further management if the,
- respiratory distress persists for ≥ 4 hours or worsens
- oxygen requirements increase over this time.
This re-evaluation involves,
- reassessment of the diagnosis and management
- repeat of the Respiratory Score if spontaneously breathing
- optimization of oxygenation
- optimization of respiratory support
- re-entry into the ACoRN Process
As a reminder that Infection often presents with respiratory symptoms in the newborn, all three Respiratory Alerting Signs are ACoRN alerting signs with *.
- Term babies with mild respiratory distress should enter the Infection Sequence only if they exhibit one or more of,
- o respiratory distress ≥ 4 hours after birth
- o risk factors for infection
- o clinical deterioration (for example, an increase in oxygen requirements)
- o requirement for ventilatory support
- All preterm babies with any degree or duration of respiratory distress should enter the Infection Sequence and receive antibiotics.
You change the existing check mark in the second box of the Alerting Signs for Infection for a question mark, to remind you to reassess within 4 hours if the baby will need to enter the Infection Sequence.
Over the next hour, the nurse reports that the baby is no longer grunting, has a respiratory rate of 50/minute, and is alert and active. The supplemental oxygen is gradually decreased while the SpO2 is continually monitored. At the end of the hour, the baby has a saturation of 93% in room air.
Respiratory Case # 2 – Respiratory distress in a preterm newborn – Initiating CPAP #
A 2240 gram baby boy is born at 34 weeks gestation by spontaneous vaginal vertex delivery following a pregnancy complicated by rupture of the membranes and preterm labor. The baby cried at birth and required minimal resuscitation. The Apgar score was 7 at 1 minute and 8 at 5 minutes.
After initial resuscitation, he develops regular but labored respiration, audible grunting at rest, and sternal retractions. The respiratory rate is 72/minute, and the heart rate 160 bpm. He requires oxygen to remain pink.
Cyanosis or oxygen requirement is an Alerting Sign for immediate resuscitation.
You work through the Core Steps of the Resuscitation Sequence. The respiratory rate remains regular and the heart rate 156 bpm. You then exit the Resuscitation Sequence and complete the ACoRN Primary Survey.
The baby is in the special care nursery area of your community hospital. He is under a radiant warmer with servo control receiving 35% oxygen by oxygen hood. The pulse oximeter reading is 92%. The respiratory rate is 72/minute and heart rate 160 bpm. The blood pressure by cuff is 48/30, mean of 36 mmHg, which is normal for a baby of 34 weeks gestation.
You observe the baby and notice he is pink, and is lying in a semi-flexed posture characteristic of a baby of his gestational age. He continues to grunt at rest, and has moderate sternal retractions and intercostal indrawing. You auscultate his chest and find that breath sounds are decreased bilaterally.
Your Primary Survey generates a Problem List that indicates that there are three areas of concern
You enter the Respiratory Sequence and carry out the Core Steps and calculate the ACoRN Respiratory Score:
The ACoRN Respiratory Score adds up to 7, indicating moderate respiratory distress and that respiratory support may be needed.
Continuous positive airway pressure (CPAP): The administration of continuous positive airway pressure (CPAP) during spontaneous breathing stabilizes the small airways and chest wall, and prevents atelectasis at end expiration. CPAP decreases the need for endotracheal intubation and mechanical ventilation in babies with moderate respiratory distress and good respiratory effort.
CPAP must only be administered and monitored by on-site and trained personnel, in a setting with adequate resources for the care of a baby needing respiratory support.
The purpose of CPAP is,
- to improve arterial PO2 in order to reduce inspired oxygen concentration in babies with respiratory distress who do not require mechanical ventilation
- to wean the baby from mechanical ventilation
- to treat apnea in some preterm babies
- o CPAP reduces mixed and obstructive apnea, but has no effect on central apnea.
CPAP is contraindicated in babies,
- in respiratory failure
- incapable of spontaneous breathing efforts (for example, central nervous system disorders)
- who are easily agitated or do not tolerate CPAP
- where excessive air swallowing is undesirable
- o gastrointestinal obstruction
- o necrotizing enterocolitis
- o congenital diaphragmatic hernia.
CPAP can be delivered using,
- nasal prongs
- nasal masks
- nasopharyngeal tube.
CPAP can be generated by,
- ventilators on CPAP mode
- circuits with free flow of gas exiting through an underwater seal (“bubble CPAP”) or valve
- infant flow drivers
- a flow inflating bag and mask (transiently).
Continuous positive airway pressure (CPAP) #
You decide to initiate nasal CPAP because the baby has moderate respiratory distress. There is on-site personnel who are familiar with CPAP and the hospital has adequate resources to care for a baby needing respiratory support.
Vascular access is started via a peripheral vein and a chest radiograph is ordered. Venous blood is drawn for a blood gas, CBC, glucose and blood culture.
- Vascular access is needed to administer fluids and medications.
- A chest radiograph is requested to diagnose lung pathology, such as TTN or RDS, or complications, such as pneumothorax.
- Blood gases are drawn to assess the adequacy of ventilation and the presence of acidosis.
- The need for internal or external consultation is decided on the basis of the availability of resources needed to care for the baby on a continuous basis.
The mother is a 24-year-old primigravida with an unremarkable past medical history and family history. She had an uneventful pregnancy until the onset of labor at 34 weeks. On admission, her cervix was 7 cm dilated and contractions were occurring every 3 minutes. In discussion with the regional centre, it was decided that transfer would be unsafe as delivery was imminent. Intrapartum antibiotic prophylaxis was suggested, and one dose of Penicillin G was given shortly after admission, about four hours before birth. Membranes had ruptured 5 hours before birth.
Currently the baby is on CPAP of 5 cmH2O, 40% oxygen, and the SpO2 is stable around 92%. Respiration is less labored and the respiratory rate 60/minute. Heart rate, blood pressure, and temperature remain within normal limits. The chest radiograph is shown below
In view of the history, physical examination, and chest radiograph findings, a presumptive diagnosis of moderate to severe TTN is made. It is likely that there is some loss of lung volume in the bases, making the hemi-diaphrams difficult to see.
At this time you exit the Respiratory Sequence, returning to the ACoRN Problem List in order to address Fluid & Glucose Management and Thermoregulation; and there are several Alerting Signs with an *, indicating that you will also have to address the Infection Sequence.
Once CPAP has been initiated, ongoing assessment is necessary to optimize oxygenation and the level of respiratory support. In a spontaneously breathing baby this is done through,
- reassessment of the Respiratory Score
- measurement of blood gases
- continuous assessment of oxygenation using pulse oximetry (SpO2)
Blood gases
pH estimates the blood total acid load, which mostly reflects dissolved CO2 but may also include metabolic acids such as lactic acid.
PCO2 indicates how well the lung is removing CO2 from the blood (ventilation).
PaO2 (arterial PO2) indicates how well the lung is transferring oxygen to the blood (oxygenation) in relation to % inspired oxygen.
Base deficit, BD, estimates how much metabolic acid is present in the blood. Base excess (BE), the negative value of BD, and bicarbonate are also used to describe the acid-base status.
Arterial, capillary or venous samples are nearly equally useful for the determination of PCO2, pH and base deficit.
SpO2 can be used as a continuous estimate of oxygenation.
Blood gases are considered satisfactory in acute respiratory illness when the pH is 7.25 to 7.40 and PCO2 45 to 55 mmHg.
The presence of an acidosis (pH ≤ 7.25) with PCO2 ≥ 55 is an indication of poor ventilation (respiratory acidosis).
Blood gas interpretation #
You decide that the blood gas result is satisfactory, the pH is between 7.25 and 7.40 and PCO2 45 to 55 mmHg. You note the baby’s grunting now occurs only with stimulation. You reassess the Respiratory Score.
Respiratory Case # 3 – Respiratory distress in a preterm newborn – Initiating mechanical ventilation #
An 1800 gram baby boy is born at 32 weeks gestation by Cesarean section following antepartum bleeding because of a placenta previa. The baby developed respiratory distress at birth and was given oxygen and CPAP using a flow-inflating bag and mask in the delivery room and during transfer to the nursery for stabilization. The Apgar score was 7 at 1 minute and 8 at 5 minutes.
On admission to the nursery, the baby has regular but laboured respiration, audible grunting at rest, and marked sternal retractions. The respiratory rate is 80/minute, and the heart rate 160 bpm.
Cyanosis or oxygen requirement is an Alerting Sign for immediate resuscitation. Breathing is laboured but effective. Heart rate is > 100 bpm.
You work through the Core Steps of the Resuscitation Sequence. The respiratory rate remains regular and the heart rate approximately 160 bpm. You exit the Resuscitation Sequence and complete the ACoRN Primary Survey.
Your Primary Survey generates a Problem List that indicates that there are three areas of concern: Respiratory, Fluid & Glucose Management, and Thermoregulation.
The baby is now in the special care nursery under a radiant warmer with servo control. He is receiving 55% oxygen according to the oxygen blender, and CPAP using a flow-inflating bag and mask system. The respiratory rate is 72/minute. The pulse oximeter reads 92%. He is pink, but continues to grunt at rest, has moderate sternal retractions and intercostal indrawing. You auscultate his chest and find that breath sounds are decreased bilaterally. Non-invasive blood pressure is 48/30 and the mean 36 mmHg (normal range). The heart rate is 160 bpm. The baby’s axilla temperature is 36.5oC.
You enter the Respiratory Sequence and carry out the Core Steps and calculate the Respiratory Score.
The ACoRN Respiratory Score total is 8, indicating moderate respiratory distress and that respiratory support may be needed.
According to the Respiratory Sequence, you should consider or adjust respiratory support for babies with moderate respiratory distress. Administration of oxygen without respiratory support is also an option in moderate respiratory distress, however this increases the risk of gradual deterioration in pulmonary function due to progressive atelectasis.
Respiratory support can be provided as CPAP or mechanical ventilation.
The baby is already receiving CPAP by face mask. However, that is usually not a long term option. You must now decide how you will continue administering CPAP or whether you should initiate mechanical ventilation
I. What criteria must be met to consider a baby suitable for CPAP?
You have the resources needed to initiate CPAP or mechanical ventilation, however keeping a baby in house who is receiving respiratory support is beyond the capability of your hospital.
You request that the baby be transported to a facility where ongoing ventilation is available. In preparation for transport, you then intubate the baby with a 3.0 ETT and initiate mechanical ventilation. You remain in periodic telephone contact with the transport coordinator.
Premedication Before Elective Intubation #
Laryngoscopy and intubation are painful procedures that can provoke detrimental responses such as hypertension, increased intracranial pressure, bradycardia, and hypoxia. The goals of premedication are to provide analgesia and to blunt undesirable hemodynamic consequences. Ideally, a premedication regimen includes a combination of opiates (e.g. morphine or fentanyl), atropine, and a short acting paralyzing agent (e.g. succinylcholine). A paralyzing drug should only be administered by personnel familiar with its use and who are skilled in neonatal intubation.
In view of the discomfort and physiologic responses associated with intubation, newborns should be premedicated when possible. Intubation should not be delayed for IV access and premedication in babies requiring urgent or emergent intubation (e.g. during resuscitation).
Premedication for intubation #
Mechanical Intubation #
The administration of mechanical ventilation (cycled positive pressure) with positive end expiratory pressure (PEEP) stabilizes the small airways and chest wall, prevents atelectasis at end expiration, and re-expands the lung during inspiration.
Mechanical ventilation is delivered via an endotracheal tube,
- manually (for example, with a flow inflating bag) or
- mechanically, using a ventilator.
The indications for ventilation include,
- ineffective respiration with decreased respiratory drive (irregular breathing or apnea)
- severe respiratory distress (ACoRN Respiratory Score > 8)
- moderate respiratory distress (ACoRN Respiratory Score 5 to 8) with unsatisfactory blood gases (pH ≤ 7.25 and PCO2 ≥ 55) or inability to oxygenate despite CPAP
- as an alternative to CPAP in babies requiring transport.
Mechanical ventilation must be administered and monitored by on-site and trained personnel in a setting with adequate resources for the care of a baby needing respiratory support, or until the baby can be transported out.
Mechanical ventilation
End tidal CO2 detector
The Transport Coordinator suggests you obtain vascular access using a
- peripheral intravenous or
- an umbilical venous catheter
Vascular access using an umbilical venous line inserted 2 to 3 cm under the skin level, and secured using a silk suture to the remaining umbilical stump allows for short-term blood sampling and infusion of fluids and medications.
Emergency venous access: Umbilical vein catheterization #
You obtain a chest radiograph and venous blood for a blood gas.
You proceed to obtain a focused history and physical examination and review the results of the diagnostic tests requested.
The mother is a 28-year-old in her second pregnancy with an unremarkable past medical history and family history.
She was admitted to hospital 2 days prior for vaginal bleeding. An ultrasound had shown a low placenta and no evidence of abruption. The amount of bleeding increased this morning. A Cesarean section was performed for this reason after discussion with the regional perinatal centre.
The baby is now receiving mechanical ventilation using a time-cycled, pressure limited ventilator, with pressure of 20/5, rate of 40, and inspiratory time of 0.4 seconds. Oxygen concentration has been weaned to 40% based on pulse oximetry. The SpO2 is stable around 92%.
The baby appears comfortable. The heart rate, blood pressure, and temperature remain within normal limits. The chest radiograph is shown below.
You interpret the chest radiograph as showing reduced lung volumes with a bilateral grainy or “ground glass” appearance. You also note some air bronchograms on the right side extending past the cardiac silhouette, and that the borders of the diaphragm and heart are obscured
The endotracheal tube is in the mid trachea (arrow), appropriately above the carina.
In view of the history, physical examination, and chest radiograph findings, a presumptive diagnosis of respiratory distress syndrome is made.
You exit the Respiratory Sequence, returning to the ACoRN Problem List in order to address Fluid & Glucose Management and Thermoregulation.
You note that there are several Alerting Signs with an *, indicating that you will also have to address the Infection Sequence.
You continue the Specific Management of the Respiratory Sequence for RDS.
Respiratory distress syndrome (RDS) #
RDS is a condition caused by lack of pulmonary surfactant, a soapy material that is normally present in mature lungs. Surfactant reduces the surface tension within the alveoli, preventing their collapse and allowing them to inflate more easily.
In the absence of surfactant, there is widespread atelectasis (alveolar collapse) resulting in decreased lung volume and increased work of breathing. The lung surface area for gas exchange is reduced, resulting in hypoxemia and hypercarbia.
Symptoms usually appear shortly after birth and become progressively more severe. RDS commonly affects preterm babies and is rare in full-term babies.
The treatment of RDS is aided by the administration of exogenous surfactant.
Surfactant should be given as early as possible in babies with RDS.
- The early use of surfactant has been shown to reduce mortality, pneumothorax and other complications of RDS
- Surfactant also improves pulmonary function in babies with meconium aspiration syndrome, however,
- the decision to administer surfactant in babies with MAS should be taken with great caution as these babies may deteriorate due to labile pulmonary hypertension.
How is Surfactant Utilized? #
Exogenous surfactant is given directly into the trachea and bronchial tree via the endotracheal tube as shown in the diagram below. The usual dose (depending on the type or brand) is 4 to 5 mL/kg.
During surfactant administration, many babies desaturate and become transiently bradycardic due to brief obstruction of the airway.
- This usually resolves with positive pressure ventilation
- Sometimes the ventilator settings and the % inspired oxygen need to be increased temporarily
- If desaturation and bradycardia persist, it may be necessary to slow or halt the administration until the baby improves.
Following surfactant administration, as lung inflation improves, the pressures required to inflate the lungs (produce an easy rise of the chest) and % inspired oxygen required often drop dramatically. It is important to,
- closely monitor changes in oximetry readings and serial blood gases
- reduce the peak ventilator pressures as needed to avoid complications of over inflation, including pneumothorax
- reduce the % inspired oxygen to maintain SpO2 in the desired range.
An improvement in respiratory status may be temporary and does not eliminate the need for transport to a center capable of a higher level of neonatal care.
Health care providers administering surfactant must be skilled in neonatal intubation and be prepared to deal with the rapid changes in lung compliance and oxygenation during and after surfactant is given. They must also be aware of the potential complications of this treatment.
Surfactant #
Post surfactant administration the baby is comfortable in 25% oxygen with SpO2 of 93%.
The umbilical venous blood gas result is: pH 7.30, PCO2 45, PO2 30, BD 3.
You are satisfied that blood gases show a pH between 7.25 and 7.40, and that the PCO2 is between 45 and 55 mmHg. You disregard the venous PO2 as the SpO2 offers a more accurate assessment of oxygenation.
You decide to continue providing mechanical ventilation, paying close attention to the baby’s clinical status while awaiting the arrival of the transport team.
Continuous oximetry will be used as your main guide to escalate or wean oxygen therapy, and blood gases will be repeated every 4 to 6 hours if the baby remains stable. You decide that blood gases will be repeated sooner if there is deterioration in the baby’s respiratory status such as increased oxygen requirements > 10 to 20%.
At 4 hours of age, the transport team arrives.
The baby’s oxygen requirements have remained at 25% with SpO2 92%. A new blood gas has shown that pH and PCO2 remain within the desired range. Ventilation settings are: pressure of 20/5, rate of 40/minute, and inspiratory time of 0.4 seconds.
Two days later, you hear that the mother and baby are doing well. The baby is no longer on a ventilator, and feeds are advancing.
Respiratory Case # 4 – Sudden deterioration in a ventilated baby #
You are waiting for the transport team to transfer a 1500 gram baby girl, born at 30 weeks gestation, who developed respiratory distress at birth and required intubation, mechanical ventilation and surfactant.
The baby was born 2 hours ago to a mother who presented in active labor, near full dilatation, after a short labor. Intrapartum and post-partum, her temperature was 38oC, and she has been treated with antibiotics for suspicion of chorioamnionitis possibly due to an amniotic fluid leak of 24 hours.
You have worked through all the areas of concern in the ACoRN Primary Survey and the Infection Sequence.
The baby is on a radiant warmer with servo control, and has an umbilical venous catheter for short-term infusions and blood sampling. Pulse oximetry reads 92% and an umbilical venous blood gas, obtained one-hour ago, showed pH 7.34, and PCO2 45 mmHg on 40% oxygen on ventilator settings of 20/5, rate of 50, and inspiratory time of 0.4 seconds.
As you return to complete your charting after talking to the parents, the nurse tells you that the oxygen requirements have rapidly increased from 40% to 100% in the last 5 minutes and that the baby is “fighting against the ventilator”.
You ask the nurse for assistance and rapidly assess the baby using the Alerting Signs of the Resuscitation Sequence. The ventilator is cycling as preset, and air entry can be heard on auscultation of both lungs; the baby is on 100% oxygen, looks pink but mottled and her SpO2 is 92%. The heart rate on the monitor and by auscultation is 180 bpm.
Your reassessment indicates the baby needs no resuscitation.
You proceed to the ACoRN Primary Survey.
The Primary survey identifies two areas of concern: Respiratory and Cardiovascular. The blood pressure is 40/22 with a mean of 30, which is in the normal range for this baby. Fluid & Glucose Management and Thermoregulation have been monitored regularly and not been a problem.
You enter the Respiratory Sequence.
You check if the airway is patent.
Airway patency
Checking for airway patency in an intubated baby includes ensuring that the endotracheal tube (ETT) is not,
- kinked
- obstructed by secretions
- displaced from proper position (baby extubated or tube too far in).
Ensuring that the endotracheal tube is not displaced from its proper position involves,
- making certain that it is at the same cm mark as when inserted
- using an end-tidal CO2 detector to determine if the tube is in the trachea
- auscultating for presence and symmetry of breath sounds in chest but not over the stomach area (may not be a reliable sign in small babies)
- inspecting the tube position using a laryngoscope.
End-tidal CO2 detector #
You inspect the endotracheal tube ensuring it is not kinked, and suction for scant amount of loose white secretions. You ensure that the endotracheal tube is not displaced from its proper position. You note that the colorimetric sensor of the end-tidal CO2 detector is changing color with each exhalation.
The baby is already receiving 100% oxygen.
You quickly ensure all monitors are properly placed, but do not calculate the Respiratory Score as the baby is receiving mechanical ventilation.
You proceed to optimize ventilation.
Optimize ventilation
Optimizing ventilation involves ensuring that,
- the baby is connected to the ventilator
- the ventilator is delivering the settings indicated and is not malfunctioning
- o check equipment while providing manual ventilation
- chest expansion can be observed and breath sounds are equal and symmetrical
- baby is breathing in synchrony with the ventilator
- pulse oximetry and blood gases are within the target range
- o SpO2 88 to 95%
- o pH 7.25 to 7.40 and PCO2 40 to 55 in a capillary, venous or arterial gas.
You ensure that the ventilator is properly connected to the baby and is not malfunctioning, observe that there is chest expansion and hear bilateral breath sounds. The baby already has a peripheral intravenous line and an umbilical venous catheter in place.
You prepare to obtain an umbilical venous blood gas and request a chest radiograph.
The nurse tells you the baby deteriorated rapidly over the last 5 minutes, needing an increase in oxygen concentration from 40% to 100% in order to maintain a SpO2 approximately 90% and that bilateral air entry could be heard.
The baby remains mottled. The heart rate is 188 bpm, and the precordium is very active but does not appear to be displaced.
What can cause a sudden deterioration in a ventilated baby?
As you followed the Sequence you have been able to troubleshoot the causes for acute deterioration in a ventilated baby. However, the acronym D.O.P.E. is useful in remembering potential causes:
D…displaced endotracheal tube? Has the baby accidentally extubated or is the endotracheal tube too far in?
O…obstructed airway or endotracheal tube?
P…pneumothorax or other critical diagnosis? Other causes may include pulmonary interstitial emphysema or atelectasis.
E…equipment working and ventilation optimized?
You decide the working diagnosis needing to be ruled out at this time is the presence of a pneumothorax.
Pneumothorax
A pneumothorax occurs when there is regional or global overdistension of the lung leading to rupture of alveoli or terminal bronchioles and release of intrapulmonary air into the pleural space.
A pneumothorax may occur when there is,
- rapid improvement in lung compliance after surfactant therapy
- excessive airway pressure
- plugging of small airways causing a ball-valve effect.
A “spontaneous pneumothorax” is one that occurs in spontaneously breathing babies, usually around the time of initial lung inflation.
Babies who are at high risk of pneumothorax include those,
- with RDS, MAS or hypoplastic lungs
- receiving respiratory support, especially mechanical ventilation.
The risk of pneumothorax is highest in the first 24 to 48 hours after birth.
How is a pneumothorax diagnosed?
1. Chest radiograph: A chest radiograph is the definitive test to diagnose a pneumothorax.
2. Chest transillumination: Comparative transillumination of the chest may be useful when a baby is deteriorating rapidly and a chest radiograph cannot be obtained in a timely fashion. Transillumination is less sensitive when used in term and near term babies.
Transillumination must be done in a darkened environment using a fiberoptic device capable of delivering high illumination.
- The fiberoptic device must be in direct contact with the baby’s chest.
- A unilateral pneumothorax is suspected when the halo around the point of contact is significantly larger on one side of the chest compared to the other.
Pneumothorax – Chest transillumination #
You review the chest radiograph.
Management of a symptomatic pneumothorax
A symptomatic pneumothorax, especially one under tension, needs to be drained urgently and takes precedence over exiting the Respiratory Sequence to complete the Problem List.
There are two ways to drain a pneumothorax: chest tube insertion or needle aspiration.
1. Chest tube insertion:
The insertion of a chest tube provides continuous drainage of a pneumothorax, allowing re-expansion of the ipsilateral collapsed lung and release of pressure on the heart and other mediastinal structures.
A chest tube should never be left open to the environment,
- this would allow air to be drawn back into the pleural space with spontaneous respiratory effort.
To prevent air re-entry, before unclamping the chest tube it should be connected to,
- a drainage system with an underwater seal, or
- a Heimlich flutter valve if preparing the baby for transport.
Initial indications that a chest tube is within the pleural space are,
- palpation of the tube between the ribs rather than up the chest wall, just after the tube insertion
- bubbling into the underwater seal at the time of unclamping
- appearance of condensation and serous drainage in the tube
- fluid meniscus moving along the tube
- improvement of the baby’s oxygenation and perfusion.
Drainage of frank blood is unusual and may indicate that a blood vessel has been disrupted (e.g. intercostal artery).
Definitive confirmation that the chest tube placement is intrapleural and the pneumothorax is drained is by chest radiograph.
Pneumothorax – Chest tube insertion #
2. Needle aspiration:
This procedure should only be undertaken as an emergency in a baby with significant compromise and a positive transillumination or chest radiograph.
- In severely symptomatic babies it may be necessary to proceed with needle aspiration prior to a confirmatory chest radiograph after ensuring the endotracheal tube has not been displaced or obstructed.
Needle aspiration is usually an interim measure pending placement of a chest tube.
The needle can be held in place for ongoing removal of air or be connected to an underwater seal.
Pneumothorax – Needle aspiration #
You insert the needle through the second intercostal space, just above the third rib, over the midclavicular line, and remove 50 mL of air. The SpO2 improves to 95% and she looks less mottled. Gradually, the oxygen is weaned to 60%. The heart rate is now 165 bpm and the blood pressure 42/28 mmHg (mean is 34 mmHg).
The nursery staff prepares equipment for the chest tube insertion. An assistant holds the needle in place and aspirates intermittently, using a stopcock, to withdraw any re-accumulation of air.
You exit the Respiratory Sequence and return to the Problem List. As you enter the Cardiovascular Sequence you note the baby’s perfusion and blood pressure have normalized and the baby no longer meets the alerting signs.
Because antibiotics were initiated 2 hours ago you do not need to re-enter the Infection Sequence.
You proceed to insert a chest tube. After the chest tube is inserted you see condensation in the tube along with a small amount of serous fluid. The chest tube is sutured in place and attached to an underwater drainage system.
A chest radiograph is ordered to check the position of the chest tube and to ensure the pneumothorax has been drained.
You can now assess and optimize oxygenation and ventilation by repeating the blood gases and adjusting the amount of oxygen being delivered and the ventilator settings.
When the transport team arrives the baby is stable on 50% oxygen and the ventilator settings have been weaned.
Several hours later, you hear from the admitting physician that the baby and mother have arrived in good condition.
Respiratory Case # 5 – Meconium aspiration #
You are called to the Cesarean delivery of a baby at 41 weeks and 3 days gestation. There is copious meconium noted at birth and the baby is not vigorous. Following resuscitation guidelines, the baby is carried to the radiant warmer and is endotracheally suctioned twice for moderate amounts of thick green meconium.
The baby requires positive pressure ventilation and chest compressions before the heart rate rises above 100 bpm at 2 minutes of age. Recovery of heart rate is followed by respiratory effort and improvement in color by 4 minutes. Tone and reflex irritability are beginning to improve by 6 minutes of age. The assigned Apgar score is 1, 5 and 8 at one, five and ten minutes respectively.
Post resuscitation the baby is pink with free flow oxygen by face mask and has labored respiration with nasal flaring, retractions and grunting. Respiratory rate is 90/minute, heart rate 156 bpm, BP 64/41 mmHg, and axillary temperature 36.3oC.
You determine that the baby shows no resuscitation signs for immediate resuscitation now and proceed to complete the ACoRN primary survey to generate the problem list.
You enter the Respiratory Sequence and carry out the Core Steps.
The baby is already on a radiant warmer with servocontrol, in an oxygen hood with 45% oxygen, and monitors are attached. The SpO2 reads 90%.
You calculate the Respiratory Score.
The Respiratory Score adds up to 7, indicating moderate respiratory distress and that respiratory support may be needed.
You ask the Respiratory Therapist to start nasal CPAP of 5 cm H2O, and request a chest radiograph.
You also prepare to insert an umbilical venous catheter in order to have intravenous access and obtain blood for a blood gas. A blood glucose determination is needed to complete the Primary Survey.
Based on the presenting history and signs of respiratory distress you are concerned that the baby may have aspirated meconium, and decide to obtain a consult alerting your regional transport coordinator.
Your focused physical examination shows the baby is receiving CPAP 5 cm H2O and 45% oxygen. The respiratory rate is 76/minute, heart rate 154 bpm, and blood pressure 58/32 mmHg (mean 46). The oxygen saturation is 92%.
You note he is a well grown, post dates male weighing 3890 grams. He is centrally pink with acrocyanosis. Meconium staining is noted in the skin creases and around his umbilical cord. There are no dysmorphic features or other abnormalities found on physical examination.
Satisfied that he is stable for the present, you go to the parents to obtain a focused history and inform them of their baby’s current condition and the management plans.
Mother is a healthy 32-year-old whose pregnancy was uneventful. The maternal serum screen and screening ultrasounds were normal and GBS swab was negative at 36 weeks. Labor was induced due to post dates. Membranes were ruptured artificially 6 hours prior to birth at which time meconium was noted. Electronic fetal monitoring was non-reassuring during the second stage and a caesarean section was performed.
The admission chest radiograph is shown on the next page.
Having established a working diagnosis, you move to address the rest of the ACoRN Problem List to address Neurology, Fluid & Glucose Management and Thermoregulation.
You note that in the Primary Survey there are four Alerting Signs with * which necessitate entering the Infection Sequence. You would initiate antibiotic therapy as this baby is receiving respiratory support and respiratory distress is unlikely to resolve by 4 hours of age.
Babies with respiratory distress should be treated with antibiotics after obtaining blood cultures.
- Early sepsis and pneumonia are indistinguishable clinically and radiologically from other forms of respiratory distress.
You enter the Specific Management section of the Respiratory Sequence.
What is Meconium Aspiration Syndrome (MAS) #
In MAS, respiratory distress is secondary to the aspiration of meconium.
Respiratory distress in MAS can be mild and transient, or severe leading to respiratory failure with hypoxemia, acidosis and persistent pulmonary hypertension (PPHN). MAS always warrants close observation as even babies who are initially stable can deteriorate quickly and develop refractory PPHN
Aspiration of meconium has three main effects on pulmonary function,
- airway obstruction
- surfactant inactivation
- chemical pneumonitis.
Because MAS is a disease that begins with fetal compromise in utero, it appears that most cases are not preventable with interventions at birth, such as endotracheal suctioning.
The main complications of MAS are,
- respiratory failure
- PPHN
- pulmonary air leaks, especially pneumothorax.
1. Avoiding respiratory failure #
The best strategy to avoid respiratory failure is to maintain optimal lung inflation and prevent atelectasis.
- In babies with moderate respiratory distress associated with MAS, this is best accomplished using CPAP.
2. Avoiding PPHN #
PPHN is a pulmonary vascular disorder that may have its onset in utero. The mechanisms for its development are not fully understood.
The pulmonary arterioles may show,
- increased muscularization
- increased contraction and reactivity
- decreased responsiveness to endogenous vasodilating stimuli
- increased responsiveness to endogenous vasocontrictive stimuli
In addition, babies with CDH and lung hypoplasia have decreased airway and pulmonary arteriolar branching.
Interventions that help decrease the pulmonary arterial pressures during or following transition in babies prone to PPHN include,
- minimizing handling and disturbance
- maintaining oxygenation in the high end of the normal range
- PO2 70 to 90 mmHg, and SpO2 approximately 95%
- minimizing atelectasis while avoiding overdistension in babies with moderate to severe respiratory distress
- CPAP
- surfactant therapy
- mechanical ventilation
- avoiding and correcting respiratory and metabolic acidosis to maintain initially
- pH 7.30 to 7.40
- PCO2 40 to 50 mmHg.
Once established, PPHN is very difficult to treat.
Avoiding pumonary air leaks #
The best strategy to avoid pulmonary air leaks is to prevent lung overdistension. For babies receiving mechanical ventilation, this is best accomplished by,
- avoiding overdistension by limiting levels of CPAP to 5 to 6 cmH2O
- avoiding overventilation (PCO2 < 35 mmHg)
- administering surfactant
- suctioning the ETT when needed.
Inspired oxygen concentration remains at 45%, and at SpO2 95%. The umbilical venous blood gas results show pH 7.28, PCO2 52, PO2 30, BD 2.
The hemoglobin is 162 g/L, WBC 22.1 x 109 /L and platelets 216 x 109 /L.
Blood glucose is 2.9 mmol/L.
You reassess and optimize oxygenation and respiratory support, and repeat the Respiratory Score.
Baby remains tachypneic with moderate sternal and intercostal retractions and nasal flaring. His grunting is less prominent than prior to starting CPAP. Air entry is equal bilaterally but crackly and diminished at the bases. The ACoRN Respiratory Score is now 5.
After reassessing the ACoRN Respiratory Score and blood gases, you decide the baby is managing well on CPAP, and it is not necessary to consider escalation of therapy with mechanical ventilation at this point.
Additional Treatments and Information about MAS #
Mechanical ventilation in MAS
Mechanical ventilation is usually reserved for babies with,
- oxygen requirement > 60% to maintain SpO2 > 90%,
- PCO2 > 55 or pH < 7.25.
However,
- the acts of intubation and initiation of mechanical ventilation can cause a baby with MAS to react adversely and PPHN to worsen
- o this complication may be decreased by use of premedication for intubation, and sedation during mechanical ventilation
- babies with MAS often have low lung compliance, and require high ventilation pressure (> 25 to 28/5 cmH2O)
- o muscle paralysis may become necessary to achieve control of ventilation and oxygenation.
Surfactant therapy
Meconium aspiration causes secondary surfactant deficiency. Clinical trials have shown that surfactant replacement therapy is beneficial in MAS. However, surfactant must be administered cautiously, avoiding hypoxia and excessive stimulation with negative effects on the labile pulmonary circulation.
As you wait for the transport team to arrive, you discuss with the staff in the nursery other considerations that are important when stabilizing a baby with MAS.
Blood pressure and intravascular volume
Babies with MAS and PPHN may have a pulmonary arterial pressure that exceeds their systemic blood pressure. This leads to right to left shunting through the ductus arteriosus, and post-ductal hypoxemia.
When right ventricular pressure is supra-systemic, the amount of blood pumped by the heart may decrease (right ventricle failure). The right atrial pressure increases leading to right to left shunting through the foramen ovale.
These babies also third-space considerable amounts of intravascular volume.
Maintenance of systemic blood pressure at least level with the pulmonary arterial pressure is important in the management of MAS with PPHN. Volume expansion and inotropic therapy may be necessary to maintain blood pressure. Dopamine is the inotropic drug most commonly used for initial therapy.
Minimizing stimulation
Babies with MAS and others predisposed to PPHN have labile pulmonary circulation, and drop their oxygenation in response to stimuli such as excessive handling, painful procedures, bright lights or loud noises.
The following interventions are useful:
- shielding the baby’s eyes from light
- speaking in a low voice, and away from the baby’s bed
- minimizing handling
- nesting
- providing adequate pain relief
- considering the need for sedation (only in a ventilated baby).
You discuss the baby’s condition with the neonatologist at the regional level III center. There are no additional management suggestions. A decision is made jointly that this baby should be transferred to the level III center as soon as possible.
You ask for that transport arrangements be also made for the mother, to minimize separation from her baby.
The transport team arrives two hours later. The baby remains in stable condition, and is now on 30% oxygen. After transferring the baby to the transport incubator and talking to the parents, the team departs indicating that they will call as soon as they arrive to at the referral hospital. They also indicate that arrangements have been made for admission of the mother to a ward in close proximity to the baby.
One week later, the mother calls to say that her baby is being discharged home in good condition.
