Description #
The goal of this unit is to continue to add to the knowledge gained from the pre-requisite courses (CCBSP-000 series, CCBSP-100 series) and help to develop clinical reasoning skills. This will enable the students to learn when it is appropriate to apply the individual skills gained in the first two courses.
Learning Objectives #
- Be able to effectively manage a complicated scenario with a variety of treatment techniques
- Demonstrate competency in skills utilized
- Be able to clinically justify the rationale for treatment provided
- Identify potential adverse effects from intervention
Case History #
A 25 year old male was involved in a MVA where he was t-boned by another car on his left side. Both cars were SUVs and the left side of his car sustained remarkable damage. Upon arrival of the EHS the patient was conscious and appropriate, but complaining of severe pain on his left thorax with ensuing difficulty breathing. The EHS placed a stiffneck collar on him, then extricated him through the side window and placed him on a stretcher for transport to the VGH Emergency Department. The patient remained coherent during the transport in the ambulance and a face mask of 60% oxygen was applied with a Sp02 of 94% and RR of 32. Intubation was not indicated but there were markedly decreased breath sounds on the left side, suggesting a pneumothorax. With the proximity to the ER and no marked cardiac compromise, the EHS team decided to hold off on inserting a chest tube. He was tachycardic with a HR of 140 and a BP of 160/60. An IV was started to enable volume resuscitation and the administration of morphine. The morphine served to decrease his obvious respiratory distress.
1. MECHANICS OF CHEST WALL MOTION:
-RESPIRATORY MUSCLES
-INTERACTION BETWEEN THE LUNG AND CHEST WALL
2 THE FLAIL CHEST:
-ETIOLOGY
-PATHOPHYSIOLOGY
-TREATMENT:
-NON-SURGICAL
-SURGICAL
3 PATHOPHYSIOLOGY AND MANAGEMENT OF PNEUMOTHORAX:
-PATHOPHYSIOLOGY
-TREATMENT
4 ACUTE RESPIRATORY DISTRESS SYNDROME:
-DEFINITION
-RISK FACTORS
-PATHOPHYSIOLOGY
-THERAPEUTIC MANAGEMENT
-LONG TERM OUTCOMES
5 PULMONARY CONTUSION
-PATHOPHYSIOLOGY
-MANAGEMENT
The Boney Chest #
Mechanics of the Chest Wall #
The chest wall is made up of the rib cage laterally, sternum anteriorly, vertebral column posteriorly and the diaphragm caudally. Movement of the chest wall by respiratory muscles generates pressure gradients between alveoli and the surrounding air. This action enables air to be moved in and out of the lungs.
Respiratory Muscles #
The diaphragm consists of 2 separate muscles joined by a central tendon. It is innervated by the phrenic nerve. The lower part of the ribcage encloses the upper part of the abdomen at FRC. The diaphragm operates like a piston with it’s up and down motion and leads to increased abdominal pressure, which pushes the ribcage up and outward.
During inhalation, the ribcage moves laterally and anteriorly. The lateral movement with elevation of the ribs is similar to a ‘bucket handle motion’. The anterior motion of the sternum is more similar to a ‘pump handle motion’. The ribcage muscles include the internal and external intercostals and the parasternal muscles. The internal intercostals are used mainly for exhalation while the external intercostals are for inhalation. The parasternal muscles also raise the sternum during inhalation. During respiratory distress other muscles can be recruited for ventilation. These are the sternocleidomastoid, pectoralis, trapezius and muscles of the vertebral column. Abdominal wall muscle contraction can be used to aid exhalation.
Interaction Between The Lung And Chest Wall #
The changes in chest wall volume are essentially identical to those of lung volume. At FRC, or resting lung volume, the outward recoil pressure of the chest wall is balanced by the inward recoil of the lung, creating a negative pleural pressure. Changes in chest wall or lung compliance can increase or decrease FRC. Normally TLC, or maximum lung capacity, is determined by increasing lung stiffness rather than chest wall recoil or inspiratory muscles. However, in Neuromuscular disease, TLC is determined by respiratory muscle weakness. This is where respiratory muscle testing proves valuable.
Flail Chest #
Etiology #
To produce a flail chest, double fractures of 3 or more neighboring ribs, or combined sternal and rib fractures are required. The result is an unstable segment of the chest wall that moves paradoxically, moving inward with inspiration and outward with expiration. The most common cause of a flail chest in adults is blunt chest trauma. In children, flail chest is less common since the chest wall is more compliant.
Pathophysiology #
A flail chest disrupts the anatomic integrity of the chest wall and significantly alters its function. The flail segment is uncoupled from the forces that promote rib cage expansion and responds to intrapleural pressure changes. Consequently, with inspiration and the decrease in intrapleural pressure, the segment moves inward. The segment then moves outward on expiration in response to the positive intrapleural pressure. If there is a decrease in lung compliance due to pulmonary contusion or atelectasis, the swings in pleural pressure are amplified and there is greater paradoxical motion of the flail segment.
The location of the flail segment may impact the magnitude of abnormal chest wall motion. A lateral flail, which is most common, is associated with greater clinical impact than posteriorly wherein the back muscles provide splinting. However, different patterns may occur, such as paradoxical motion between the rib cage and abdomen. Disordered patterns of respiratory muscle function may also contribute to the motion of the flail segment. Normal recruitment patterns may be altered because of severe chest wall pain. This may explain why some patients with a flail chest remain unstable following prolonged mechanical ventilation.
Respiratory Failure results from a combination of events, with hypoventilation and flail-induced changes in lung and respiratory muscle function being key factors. When lung contusion is also present, it significantly contributes to he pathogenesis of respiratory failure. The flail segment and associated pain are instrumental in contributing to an ineffective cough with secretion retention and respiratory muscle dysfunction (including muscle spasm and an altered recruitment pattern), Atelectasis with V/Q mismatch and shunt ensue and lead to an increased work of breathing and hypoxemia. The end result is respiratory muscle fatigue and respiratory failure.
Flail Treatment #
Non-Surgical Management #
The restoration of functional integrity of the chest wall can be achieved with conservative management or surgical intervention. However, which approach is best suited for a given patient is a difficult decision.
Conservative management includes adequate analgesia, mobilization with deep breathing and coughing, and positive pressure ventilation as indicated. Pain medication can vary from oral to epidural anesthesia, but needs to be adequate to enable effective physiotherapy treatment. Mechanical ventilation solely for the purpose of providing stability to the chest wall is no longer recommended due to the increased morbidity and mortality that is associated with it. However, the use of non-invasive positive-pressure ventilation can be very beneficial without the risk. Together with adequate analgesia it enables early mobilization and other physiotherapy interventions.
Surgical Management #
Surgical fixation of the unstable flail segment has been classically used to reduce patient ventilator time and the associated morbidity and mortality. Surgical techniques include mobilization of large chest wall flaps or stabilizing the fractured ribs with titanium plates. A few small studies suggest that surgical fixation may be superior to conservative management by reducing length of invasive ventilation, duration of ICU stay, and infection rate. However, the indications for surgical fixation are not fully defined, and further research comparing it to conservative treatment is necessary.
Pneumothorax #
Pathophysiology: #
Normally the pleural pressure is negative with respect to the alveolar pressure during the entire respiratory cycle. The pressure gradient between the alveoli and the pleural space, or transpulmonary pressure, is the result of the elastic recoil of the lung. The pleural pressure is also negative with respect to the atmospheric pressure. When a communication develops between an alveolus and the pleural space, air will flow into the pleural space until there is no longer a pressure difference. A similarly effect occurs when a communication develops between the atmosphere through the chest wall and the pleural space. The ensuing increase in pressure in the pleural space decreases the recoil pressure of the lung and expands the thoracic cavity. This rise in pleural pressure also causes a shift of the mediastinum to the contralateral side, an enlarged hemithorax, and a depressed diaphragm. When severe this results in a tension pneumothorax wherein there is a sudden deterioration in the cardiopulmonary status of the patient. This deterioration is believed to be due to a combination of a decreased cardiac output due to impaired venous return and profound hypoxia due to V/Q mismatch. Patients who are on mechanical ventilation and develop a tension pneumothorax, suffer a significant drop in cardiac output. The clinical picture associated with a tension pneumothorax is striking wherein the patient appears distressed with rapid labored respirations, cyanotic, marked tachycardia, marked hypoxemia and profuse diaphoresis. By contrast, a patient with a simple pneumothorax will present with a decrease in vital capacity and hypoxemia. In primary pneumothorax the decrease in VC is well tolerated, but in abnormal lung function states it may lead to respiratory insufficiency with significant alveolar hypoventilation.
The incidence of pneumothorax after blunt trauma depends on the severity of the trauma and has exceeded 35% in some studies. A pneumothorax may develop from a penetrating chest wall trauma wherein air enters the pleural space via the chest wall. It may also develop from non-penetrating trauma secondary to rib fractures, or may develop in response to a sudden chest compression which abruptly increases the alveolar pressure, resulting in alveolar rupture.
Treatment #
Treatment of the Pneumothorax #
Treatment of the traumatic pneumothorax is most often managed with a chest tube insertion. If the air leak persists for more than a few days, performing a thoracostomy to identify and repair the site of the air leak is considered. Where fracture of the trachea or major bronchus presents, surgical repair of the tear may be required. Similarly, if traumatic rupture of the esophagus occurs, it will also require surgical repair.
Contusion #
Pulmonary Contusion #
Pulmonary contusion is a common lesion occurring in patients sustaining severe blunt chest trauma. Alveolar hemorrhage and parenchymal destruction are maximal during the first 24 hours after injury, and then usually resolve within 7 days.
Pathophysiology of Pulmonary Contusion #
Pulmonary hemorrhage is the outstanding lesion from blunt chest trauma. The lung tissue reacts and produces more than its normal amount of interstitial and intra-alveolar fluid. The bronchopulmonary tree not only has more fluid to remove, but is also less capable of doing so. Some studies have implicated the vigorous IV fluid resuscitation as a contributing factor to respiratory problems after thoracic trauma. Researchers have stated after a 2-year study, that direct damage to the lung, rather than bony injury, was the cause of respiratory dysfunction.
Lung injury with rib cage trauma involves damage to the lung from transmission of mechanical forces to the thoracic cage, with increased tissue pressure and subsequent tearing of tissues. There may also be direct laceration of the lung by displacement of fractured ribs or chest wall compression, bleeding into uninvolved lung segments causing irritation with subsequent depression of alveolar function and bronchospasm, increased mucous production with decreased clearance, and decreased surfactant production leading to alveolar collapse.
Parenchymal lung damage leads to pathophysiologic changes that, depending on the extent and severity of the injury, can culminate in respiratory failure. These changes include ventilation-perfusion mismatch, elevated intrapulmonary shunt, increased lung water, and loss of lung compliance as a result of segmental lung damage. This clinically presents as hypoxemia, hypercarbia, and an increased work of breathing. The patient may consequently present with an increased respiratory rate, wheezes, and occasionally hemoptysis. Abnormalities on CXR may not present for 4-6 hours, and are more clearly defined on CT. Generally, this respiratory deterioration resolves in 3-5 days, unless further compromise develops from a local inflammatory response to the injured lung, systemic inflammatory responses related to associated injuries, or the development of pneumonia.
Severe pulmonary hemorrhage is a progressive lesion after pulmonary contusion. The interstitial hemorrhage is followed in 1-2 hours by interstitial edema and the infiltration of monocytes and neutrophils. After 24 hours, protein, red blood cells, and a massive accumulation of inflammatory cells are found along with fibrin in the alveoli. There is a loss of architecture and massive edema develops. 48 hours after injury, more fibrin, cell debris, granules from type II alveolar cells, and many neutrophils and macrophages are present. The lymphatics are dilated and filled with protein. Healing is almost complete after 7-10 days with little residual scarring.
Management #
Pulmonary Contusion Managment #
The current management of pulmonary contusion is supportive, including optimal pain control, and involves directing care at the exclusion of associated injuries. The patient may benefit from placing the obviously contused lung in a dependent position to prevent bleeding into the minimally injured lung. Overall, patients are intubated only if they manifest respiratory difficulties or imminent failure. Underlying pulmonary disease or associated injuries may necessitate ventilatory support in certain patients. In severe unilateral lung lesions, arterial desaturation may be minimized by placing the ICU patient on a rotating bed to optimize ventilation-perfusion matching in the ‘good’ lung. These beds have also been demonstrated to significantly reduce the incidence of pneumonia and the number of ventilator days after severe thoracic trauma. Selective bronchial intubation of patients with massive intratracheal bleeding may also aid in the treatment of severe unilateral pulmonary contusions.
Resuscitation from hemorrhagic shock has been associated with increased capillary permeability, thus increased lung water in some studies. Generally, fluid resuscitation is performed judiciously. There is little or no evidence to support the use of antibiotics and steroids in the management of pulmonary contusion.
In summary, patients are best managed by ICU monitoring with aggressive pulmonary toilet, meticulous fluid management, and control of chest wall pain with anesthetic methods such as epidural catheter infusions. This aggressive critical care management of severe chest trauma has reduced the need for intubation from 100% to only 23%, and has improved survival from 60% to 93.5%.
Outcomes #
Pulmonary Contusion Outcomes #
The severity of pulmonary contusion correlates with the development of pulmonary infections, ARDS, respiratory failure and death. The implementation of mechanical ventilation significantly decreased the number of early deaths from respiratory failure, but delayed mortality from sepsis and tracheostomy complications became marked. The advance of selective intubation was responsible for marked improvement in survival. However, where flail chest is present, the presence of pulmonary contusion significantly increases both the incidence of intubation and the associated mortality. Patients with flail chest were examined prior to discharge and at 6 months, and no residual pulmonary derangements were found. However, when associated with pulmonary contusion, there were persistent abnormalities in FRC and oxygenation. Disabling dyspnea was seen in the patients with pulmonary contusion and a flail chest, but not those with isolated flail chest. Chest CT revealed fibrosis in the pulmonary contusion patients. Overall, despite therapeutic interventions, lung contusion alone remains associated with a significant morbidity and mortality
ARDS #
1. Definition:
The acute respiratory distress syndrome or ARDS, is characterized by noncardiogenic pulmonary edema, lung inflammation, hypoxemia, and decreased lung compliance. ARDS is a syndrome which reflects a number of clinical and physiologic observations thought to represent a common pathology, for which there is no specific diagnostic test.
A consensus conference of American and European investigators published their definition of ARDS as follows:
Acute Lung Injury Pa02/Fi02 < 300 mmHg CXR bilat infiltrates
ARDS Pa02/Fi02 < 200 mmHg CXR bilat infiltrates
The bilateral infiltrates are associated with pulmonary edema.
PAWP < 18 or no evidence of left atrial hypertension in both instances. <-turn this section into a table.
However, this definition can be considered simplistic and does not reflect the response to PEEP or mechanical ventilation, in terms of degree of hypoxemia and mortality rate. As a result, the research into the incidence and management of ARDS remains unclear.
Risk Factors #
Data from several studies has shown that sepsis, aspiration, multiple blood transfusions, ulmonary contusion, pneumonia and smoke inhalation were associated with the highest risk of developing ARDS. In addition, chronic alcoholism is a predisposing factor for ARDS, although the exact mechanisms responsible are unclear.
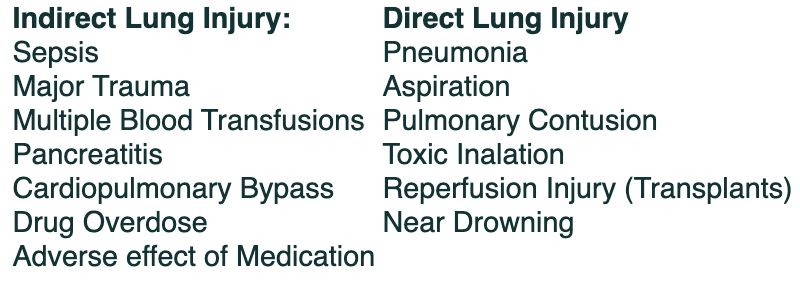
The conditions associated with ARDS have been further defined by whether they represent indirect or direct lung injury mechanisms.
Pathophysiology #
ARDS has been classically defined as noncardiogenic pulmonary edema. Whereas in CHF elevated left sided cardiac pressures cause hydrostatic pulmonary edema, in ARDS the edema is due to increased permeability of the alveolar-capillary barrier which permits leakage of protein-rich fluid into the airspaces. Alveolar filling with fluid leads to decreased compliance as well as profound hypoxemia. Although pC02 is within normal, dead-space ventilation is significantly increased. Pulmonary hypertension is also commonly observed with a number of proposed mechanisms. These include hypoxic vasoconstriction, intravascular fibrin deposit in the pulmonary capillaries, and compression of blood vessels by positive pressure ventilation.
There are three overlapping and sequential stages in the pathology of ARDS. In the first or exudative stage, diffuse alveolar damage occurs wherein there are hyaline membranes and protein-rich fluid in the alveolar spaces. There is also epithelial disruption and infiltration of the air spaces with neutrophils and macrophages. This phase is thought to last 5-7 days, and in some patients is followed by a proliferative phase wherein hyaline membranes are reorganized and areas of fibrosis are visible. Obliteration of pulmonary capillaries and deposition of interstitial and alveolar collagen may be observed, along with a decrease in the number of neutrophils and the extent of pulmonary edema. Finally a fibrotic phase occurs in patients with persistent (> 2weeks) ARDS. More recent evidence suggests that the development of fibrosis probably occurs earlier than previously thought, such that fibrotic and proliferative phases occur simultaneously.
The mortality rate for ARDS has fallen since the syndrome was first described, with a rate over 60% to 40% since 1993. Although the reasons for this improvement are unclear, better supportive care with the use of smaller tidal volumes is considered a factor.
Management #
Therapeutic Management #
The first goal of therapy in ARDS is to treat the underlying cause. Secondly the goal is to prevent complications which may occur, such as VAP and DVTs. Further to this, conservative administration of fluids, while avoiding overdiuresis and hypovolemia, after the initial 24 hours of resuscitation is safe and beneficial.
Studies on the use of corticosteroids, either early or late in the course of ARDS are controversial and thus steroids are not recommended. The use of Nitric Oxide as a vasodilator may result in initial improvement in oxygenation, but there was an increased risk of renal dysfunction and no effect on survival rates. A number of surfactant abnormalities have been described in ARDS, but whether the augmentation of surfactant is useful, remains an open question. Similarly, anti-inflammatory therapies have been ineffective in treating ARDS.
Mechanical Ventilation is the standard therapy for ARDS. However, significant trauma occurred with traditional ventilation involving high tidal volumes and PEAK/PEEP pressures. Advances in the understanding of ventilator induced lung injury have significantly affected current outcomes. CT scans have demonstrated ARDS changes to be displayed as patchy infiltrates interspersed with more normal appearing areas of lung. The tidal volume will more preferentially be distributed to the more compliant, normal areas of lung, causing overdistention and ventilator induced lung injury. Furthermore, mechanical ventilation with excessive tidal volumes can cause pulmonary edema due to increased alveolar-capillary permeability very similar to ARDS. Consequently a protective ventilation approach arose with low volumes and pressures, and ensuing permissive hypercapnia. This has impacted the appearance of barotrauma and survivability, being significantly lower in the protective group. High frequency oscillation ventilation does not have data to support a clinical advantage over protective ventilation. ECMO(extra-corpeal membrane oxygenation) wherein the blood is oxygenated outside of the body has limited evidence to support it’s use in ARDS.
Physiotherapists may be involved in proning the ARDS patient as a means to improve oxygenation and subsequently decrease Fi02. Proning enables the dorsal regions of the lungs to be better ventilated as well as improved ventilation-perfusion matching. Although proning will definitively address hypoxemia, it has not shown to differ in mortality, and is a challenging procedure to perform with the complicated equipment of an ICU patient with limited reserves.
Outcomes #
Long Term Outcomes in ARDS #
Despite the significant compromise in oxygenation and respiratory compliance, many survivors of ARDS often have near normal PFTs 6-12 months later. However, survivors continue to have important functional limitations and a decreased health quality of life for 2 years. They also demonstrate a decreased functional capacity in a 6 minute walk test, attributable to respiratory changes and muscle weakness. A study demonstrated that the lack of ICU acquired illness and rapid resolution of lung injury and multiorgan dysfunction were associated with better functional status after discharge.
Presentation on Admission to Hopsital #
Upon arrival in the Emergency Department, the patient presents as follows:
Neurological Status:
-pupils equal and reactive to light
-alert and anxious with a GCS of 14
-moving all limbs moderately to command but complains of pain with movement of their left arm and leg
-on CTL Precautions with stiff neck collar in place
-MRI pending for possible clearance of spines
Cardiovascular Status:
-suspected cardiac contusion but sternum remains intact
-remains tachycardic with a HR of 134 and BP of 156/54
-receiving 2 liters of saline to address potential for going into shock
-periphery well perfused
-no indication for vasopressor or anti-arrhthmic medication
-troponin elevated to 3.5 but considered related to cardiac contusion as 12-lead ECG is normal
-hemoglobin within normal limits
-temperature 36 degrees celsius
-urine output pending
Respiratory Status:
-CXR reveals fractured ribs 2-9 on the left with a pnemothorax and suspected pulmonary contusions
-on clinical assessment there is evidence of a flail segment
-a chest tube is immediately placed on the left but there is no current evidence of a tension pneumothorax
-the patient remains in significant respiratory distress at rest with a RR of 25
-he complains of the chest wall pain limiting his ability to breathe
-ribcage motion is abnormal with the flail segment
-respirations are shallow and involve the use of accessory muscles
-on auscultation there are decreased breath sounds, particularly on the left, but no adventitia
-their cough is weak and ineffective due to pain and altered mechanics
-ABGs on 50% HFFM are:
-pH: 7.47 p02: 82 pC02: 29 HC03: 23
-the p02/Fi02 ratio is: 82/.50 = 164 (normal value is 500)
-he is turned up to 60% HFFM to achieve a higher Pa02/Fi02 ratio
-the patient reports that he is a nonsmoker and has no history of asthma
Orthopedic:
-pelvic X-rays reveal a cracked acetabulum on the left, without displacement
-a fractured clavicle on the left is observed on the chest X-ray, without displacement
-a sling is provided for comfort
-blunt abdominal trauma is suspected and an ultrasound is done:
-there is a splenic laceration but it is considered stable and not requiring surgery
-it will be monitored
Patient’s Course in Hospital:
-the patient is given further medication to achieve better pain control with subsequent improved respirations
-the Emergency physicians place a chest tube to control the pneumothorax on the left side
-an epidural has been ordered and anaesthesia will consult the patient on the trauma unit
-with the additional pain medication the patient is less SOBAR and able to tolerate the MRI in supine
-the MRI results will be available when the patient is on the trauma unit
-with the marked improvement after pain medication and the chest-tube insertion, the team decides to
admit the patient to the trauma step-down unit as they do not feel that they will require intubation
and ICU care at this point in their course
-if the pulmonary contusions become marked or ARDS develops, ICU will be consulted
-the patient is transferred to the trauma unit for continuing care
-an arterial line was not placed in ER since the trauma unit does not take arterial lines
-MRI results become available and the CTL spines are cleared such that the collar is discontinued
-the anaesthesiologist arrives to place the epidural catheter for pain management
-the RNs will monitor the motor sensory level on a regular basis to ensure the catheter remains
in the right position
-regular manual blood pressures will be taken to ensure that the pressure hasn’t dropped
significantly as a result of the epidural
-the patient is clearly more comfortable with the epidural and much less distressed at rest
-his RR has decreased to 20 at rest
– he remains on 60% HFFM with sP02 of 96% at rest
-he will be monitored closely over the next few days for significant hypoxemia and respiratory
failure as a result of the pulmonary contusions and flail chest
-he is at high risk of developing ARDS if the contusions are significant
-you cover the trauma unit and prepare to see this patient for his first Physiotherapy intervention
Orthopaedics #
Orthopedic:
-pelvic X-rays reveal a cracked acetabulum on the left, without displacement
-a fractured clavicle on the left is observed on the chest X-ray, without displacement
-a sling is provided for comfort
-blunt abdominal trauma is suspected and an ultrasound is done:
-there is a splenic laceration but it is considered stable and not requiring surgery
-it will be monitored
CVS #
CARDIOVASCULAR:
-in a hyperdynamic state with HR 115 and BP 180/95
-heart rhythm is normal sinus tachycardia
-periphery well perfused
-Hemoglobin within normal limits
-some elevation of troponin level to 3.5, but there is no evidence of ST changes on 12-lead ECG
-no indication for vasopressor or anti arrhythmic medication
-unable to determine urine output
-temperature 36 degrees celcius
-fractured sternum present with expected cardiac contusion
Resp #
Respiratory Status:
-CXR reveals fractured ribs 2-9 on the left with a pnemothorax and suspected pulmonary contusions
-on clinical assessment there is evidence of a flail segment
-a chest tube is immediately placed on the left but there is no current evidence of a tension pneumothorax
-the patient remains in significant respiratory distress at rest with a RR of 25
-he complains of the chest wall pain limiting his ability to breathe
-ribcage motion is abnormal with the flail segment
-respirations are shallow and involve the use of accessory muscles
-on auscultation there are decreased breath sounds, particularly on the left, but no adventitia
-their cough is weak and ineffective due to pain and altered mechanics
-ABGs on 50% HFFM are:
-pH: 7.47 p02: 82 pC02: 29 HC03: 23
-the p02/Fi02 ratio is: 82/.50 = 164 (normal value is 500)
-he is turned up to 60% HFFM to achieve a higher Pa02/Fi02 ratio
-the patient reports that he is a nonsmoker and has no history of asthma
Labs #
Upon arrival in the Emergency Department, the patient presents as follows:
Neurological Status:
-pupils equal and reactive to light
-alert and anxious with a GCS of 14
-moving all limbs moderately to command but complains of pain with movement of their left arm and leg
-on CTL Precautions with stiff neck collar in place
-MRI pending for possible clearance of spines
Cardiovascular Status:
-suspected cardiac contusion but sternum remains intact
-remains tachycardic with a HR of 134 and BP of 156/54
-receiving 2 liters of saline to address potential for going into shock
-periphery well perfused
-no indication for vasopressor or anti-arrhthmic medication
-troponin elevated to 3.5 but considered related to cardiac contusion as 12-lead ECG is normal
-hemoglobin within normal limits
-temperature 36 degrees celsius
-urine output pending
Respiratory Status:
-CXR reveals fractured ribs 2-9 on the left with a pnemothorax and suspected pulmonary contusions
-on clinical assessment there is evidence of a flail segment
-a chest tube is immediately placed on the left but there is no current evidence of a tension pneumothorax
-the patient remains in significant respiratory distress at rest with a RR of 25
-he complains of the chest wall pain limiting his ability to breathe
-ribcage motion is abnormal with the flail segment
-respirations are shallow and involve the use of accessory muscles
-on auscultation there are decreased breath sounds, particularly on the left, but no adventitia
-their cough is weak and ineffective due to pain and altered mechanics
-ABGs on 50% HFFM are:
-pH: 7.47 p02: 82 pC02: 29 HC03: 23
-the p02/Fi02 ratio is: 82/.50 = 164 (normal value is 500)
-he is turned up to 60% HFFM to achieve a higher Pa02/Fi02 ratio
-the patient reports that he is a nonsmoker and has no history of asthma
Patient’s Course in Hospital:
-the patient is given further medication to achieve better pain control with subsequent improved respirations
-the Emergency physicians place a chest tube to control the pneumothorax on the left side
-an epidural has been ordered and anaesthesia will consult the patient on the trauma unit
-with the additional pain medication the patient is less SOBAR and able to tolerate the MRI in supine
-the MRI results will be available when the patient is on the trauma unit
-with the marked improvement after pain medication and the chest-tube insertion, the team decides to
admit the patient to the trauma step-down unit as they do not feel that they will require intubation
and ICU care at this point in their course
-if the pulmonary contusions become marked or ARDS develops, ICU will be consulted
-the patient is transferred to the trauma unit for continuing care
-an arterial line was not placed in ER since the trauma unit does not take arterial lines
-MRI results become available and the CTL spines are cleared such that the collar is discontinued
-the anaesthesiologist arrives to place the epidural catheter for pain management
-the RNs will monitor the motor sensory level on a regular basis to ensure the catheter remains
in the right position
-regular manual blood pressures will be taken to ensure that the pressure hasn’t dropped
significantly as a result of the epidural
-the patient is clearly more comfortable with the epidural and much less distressed at rest
-his RR has decreased to 20 at rest
– he remains on 60% HFFM with sP02 of 96% at rest
-he will be monitored closely over the next few days for significant hypoxemia and respiratory
failure as a result of the pulmonary contusions and flail chest
-he is at high risk of developing ARDS if the contusions are significant
-you cover the trauma unit and prepare to see this patient for his first Physiotherapy intervention
Course in Hospital #
Patient’s Course in Hospital:
-the patient is given further medication to achieve better pain control with subsequent improved respirations
-the Emergency physicians place a chest tube to control the pneumothorax on the left side
-an epidural has been ordered and anaesthesia will consult the patient on the trauma unit
-with the additional pain medication the patient is less SOBAR and able to tolerate the MRI in supine
-the MRI results will be available when the patient is on the trauma unit
-with the marked improvement after pain medication and the chest-tube insertion, the team decides to
admit the patient to the trauma step-down unit as they do not feel that they will require intubation
and ICU care at this point in their course
-if the pulmonary contusions become marked or ARDS develops, ICU will be consulted
-the patient is transferred to the trauma unit for continuing care
-an arterial line was not placed in ER since the trauma unit does not take arterial lines
-MRI results become available and the CTL spines are cleared such that the collar is discontinued
-the anaesthesiologist arrives to place the epidural catheter for pain management
-the RNs will monitor the motor sensory level on a regular basis to ensure the catheter remains
in the right position
-regular manual blood pressures will be taken to ensure that the pressure hasn’t dropped
significantly as a result of the epidural
-the patient is clearly more comfortable with the epidural and much less distressed at rest
-his RR has decreased to 20 at rest
– he remains on 60% HFFM with sP02 of 96% at rest
-he will be monitored closely over the next few days for significant hypoxemia and respiratory
failure as a result of the pulmonary contusions and flail chest
-he is at high risk of developing ARDS if the contusions are significant
-you cover the trauma unit and prepare to see this patient for his first Physiotherapy intervention
Physiotherapy Problem List #
PHYSIOTHERAPY PROBLEM LIST:
Cardiorespiratory:
1. Significantly compromised respiratory mechanics, thus ventilation and airway clearance.
2. Rapid deterioration in oxygenation and vital signs when patient has been moved previously. However, the
RNs report that he is markedly improved with the introduction of the epidural.
Neurological:
1. Pain control may continue to be an issue even with the epidural; additional dilaudid is available.
Orthopaedic:
1. Acetabular fracture renders them non-weightbearing on the left lower extremity, but there are no limits to
ROM or positioning.
2. Fractured clavicle will likely cause pain when supporting the chest wall. They are non-weightbearing on the
left arm and a sling is recommended.
Orthopaedics #
CVS #
Resp #
Labs #
Mobility #
Example of Effective Physiotherapy Management #
EXAMPLE OF EFFECTIVE PHYSIOTHERAPY INTERVENTION:
You arrive on the ward in the afternoon and begin by going through the patient’s chart and flowsheet which he has since he’s in the trauma step-down unit. You notice that he’s down to 50% HFFM with an average SP02 of 96%. His RR averages 21 and the nurses report that his parameters have elevated quickly when they reposition him in bed. However, they report that this has improved markedly following the insertion of the epidural for pain control. His last HR was 120 and his BP 145/76. The ABG and CXR are from emergency and you consider the ABG to be specific to that time, while the CXR may have more to contribute. On the CXR you see the rib and clavicle fractures, as well as the pneumothorax and chest-tube. The lungs are small in volume but there is no significant atelectasis at that time. You will be able to augment the CXR with your auscultation findings on examination of the patient. You note the epidural medication and that there really hasn’t been any additional pain medication required since it’s insertion.
Your treatment plan is to organize adequate support with the RNs so that you can sit the patient on the edge of the bed, without the compromised vitals seen previously with repositioning. This is the most effective way that you can optimize both the volume and distribution of ventilation, as well as airway clearance. You introduce yourself to the patient, describe what your treatment will involve as well as it’s importance, and obtain consent. You notice that the patient has a small pillow to support his chest wall with his left arm. After asking him how the pain is at rest and with movement, you ask the RN if he could have an additional dose of pain medication before undertaking such a significant amount of activity. While you are waiting for the pain medication, you check his vitals, including a BP which was taken just 5 minutes previously. You also explain to the patient the specifics of your treatment and how you and the RN will conduct it. You arrange the equipment so that the patient can sit on the right side of the bed. Once the pain medication has taken effect, while coaching the patient, you turn the patient onto their right side and sit them up, with the RN bringing their legs around. Sitting up on the right side of the bed is an optimal way to minimize the pain the patient experiences, as well as enabling him to assist with his right arm and leg. Immediately the patients RR goes to 28 with their HR at 135; and since you are holding the patient, you ask the RN to take a BP, which is elevated and not compromised by the epidural. You also note that their SP02 has dropped to 92%. You continue to coach the patient on how best to support their chest wall despite the fractured clavicle, and take slow deep breaths. They begin to settle after 10 minutes with their parameters returning to normal or pre-existing values. As the patient continues to sit there, you auscultate their chest throughout and note decreased air entry on the left and absent of adventitia. The patient did cough when they first sat up, but it was unproductive. After the patient was taking the slow, deep breaths for auscultation, you notice that their Sp02 has increased to 97%. You continue to work on the slow deep breathing and relaxation, and with time the Sp02 rises further to 99%. Upon questioning, the patient tells you that he was more anxious of what to expect with the mobilization than being in significantly more pain. He felt that the extra pain medication was helpful. After 30 minutes, you organize everyone and everything to return the patient to bed. You leave him positioned in high fowlers after your treatment and ensure that pillows are positioned to support his upper arms. You acknowledge his effort as well as the importance of continuing with the relaxed deep breathing. His pain is well managed and his Sp02 remains at 99% with his RR 15 and HR 98, and his BP 127/82.
After thanking the RN working with you, they ask you why you didn’t stand the patient once he reached the point of doing so well. You explained that this was the first time that he actively mobilized, and that you wanted to be sure of his BP with the epidural, and avoid the marked respiratory distress and compromised vitals that had been reported previously with positioning. Also, his acetabular fracture renders him non-weightbearing on the left. And most importantly you wanted to make sure that his cardiorespiratory function was improved, and that this improvement was maintained without fatigue. However, you anticipate that based on todays treatment, he may stand and perhaps pivot to a chair when you see him tomorrow. You remain acutely aware of his pulmonary contusions and the potential for further deterioration and respiratory failure, and thus you will only be able to determine tomorrow’s treatment after reassessment at that time.
Factors to Consider with Respect to your Treatment:
1. Is there any other information that you would like to know to be more effective?
2. Have you done enough for him today? What else could you do?
3. If he was unable to effectively take deep breaths because of the pain, what could you do?
4. If he reported the pain was manageable but he still wasn’t able to take deep breaths, what could you do?
5. If he had a significant amount of secretions that were mobilized but not fully cleared, what could you do?
6. If his parameters remained significantly elevated(Sp02 lower), what could you do?
References #
REFERENCES:
- Ayas NT, Zakynthinos S, Roussos C, Pare PA: Respiratory System Mechanics and Energetics. In: Murray and Nadel’s Textbook of Respiratory Medicine, 5th edn. Volume 1: Chapter 5:89-98, Saunders 2010.
- Cappello M, Legrand A, De Troyer A: Determinants of rib motion in flail chest. Am J Respir Crit Care Med: 159:886-891,1999.
- Tzelepis GE, McCool FD: The Lungs and Chest Wall Diseases. In: Murray and Nadel’s Textbook of Respiratory Medicine, 5th edn. Volume 2:Chapter 88:2073-2075, Saunders 2010.
- Light RW, Lee GL: Pneumothorax, Chylothorax, Hemothorax and Fibrothorax. In: Murray and Nadel’s Textbook of Respiratory Medicine, 5th edn. Volume 2: Chapter 74:1764-1774, Saunders 2010.
- Lee WL, Slutsky AS: Acute Respiratory Distress Syndrome. In: Murray and Nadel’s Textbook of Respiratory Medicine, 5th edn. Volume 2:Chapter 90:2104-2129, Saunders 2010.
- Cohn SM: Pulmonary Contusion: Review of the Clinical Entity. The Journal of Trauma: Injury, Infection and Critical Care. Volume 42(5):973-979, 1997.
- Richardson JD, Adams L, Flint LM: Selective Management of Flail Chest and Pulmonary Contusion. Ann Surg 196: 481-487, 1982
- Epidurals
- Gundez M, Unlugenc H, Ozalevli M, et al: A comparative study of continuous positive airway pressure(CPAP) and intermittent positive pressure ventilation (IPPV) in patients with flail chest. Emerg Med J:22: 325-329, 2009.
- Engels PT, Beckett AN, Rubenfeld GD et al: Physical Rehabilitation of the Critically Ill Trauma Patient in the ICU. Critical Care Medicine:41: 1790-1801, 2013.
- Stiller K: Physiotherapy in Intensive Care. An Updated Systematic Review. CHEST Volume 144(3):825-847, 2013.
