Description #
Anaphylaxis is an immediate and potentially life-threatening systemic allergic reaction.
After exposure to an inciting agent there is a massive release of mediators from mast cells, basophils, and possibly other cells. These mediators produce a broad spectrum of signs and symptoms involving the cutaneous, respiratory, cardiovascular, and GI systems.
Midwives must understand the pathophysiology and exercise appropriate caution to prevent introduction of an allergen.
It is critical that midwives are prepared and can recognize and respond immediately to an anaphylactic event.
Learning Objectives #
– Define anaphylaxis
– Review physiological response
– Outline risks and causitive agents associated with anaphylaxis
– Describe signs and symptoms of anaphylaxis
– Outline treatment options for immediate management of anaphylaxis
– Describe preventative strategies to avoid anaphylaxis
Definitions #
Anaphylaxis is an immediate and potentially life threatening systemic reaction. It can be either IgE (immune) or non-immune mediated.
Allergic, IgE-mediated anaphylaxis is a reaction to a protein and Involves prior sensitization to an allergen with later re-exposure, producing symptoms via an immunologic mechanism.
The non immune-mediated response is an anaphylactoid reaction. There is no prior exposure required.
Both can lead to death if not responded to immediately. They call for the same immediate medical response.
Incidence #
The true incidence is unknown.
Anaphylaxis accounts for 1% of ER visits in USA and is responsible for 500 – 1000 deaths per year there.
The real incidence may be anywhere from 8.4 to 21 per 100,000 person years.
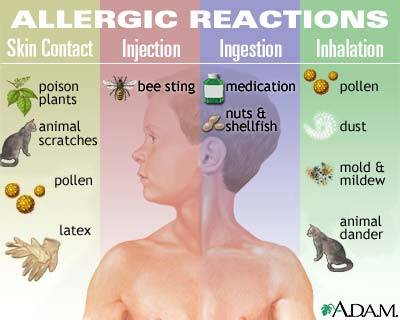
Inciting Agents
- Foreign protein is the typical inciting agent (antigen / allergen)
- Drugs
- Radiographic contrast media
- Hymenoptera stings
- Allergies: Food, Latex
- Blood products
People with a Latex allergy may also be allergic to:
- Bananas
- Kiwi
- Papaya
- Avocados
- Apricots
DRUGS
- Beta-lactam antibiotics
- Penicillins most common cause of drug-induced anaphylaxis.
- Cephalosporins
- Aspirin and other NSAIDs are the 2nd most common
- Opiates
Pathophysiology #
The response triggers a massive release of mediators from mast cells, basophils, and possibly other cells. There is an immediate release of histamine, tryptase, prostaglandins (PGD2, PGF2a), leukotrienes (LTB4, LTC4, LTD4, LTE4), and platelet-activating factor.
Hours later the same cells release cytokines. These produce broad spectrum of signs and symptoms involving cutaneous, respiratory, cardiovascular, and GI systems.
Symptoms usually present in 5 – 60 min – rarely may be delayed several hours or days after exposure.
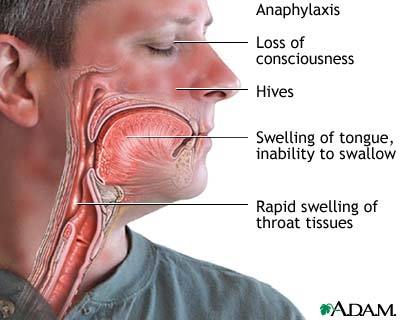
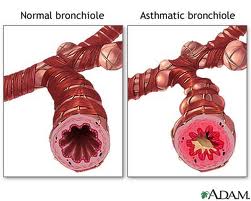
Without treatment, death results after intractable bronchospasm. Asphyxiation results from upper airway edema or cardiovascular collapse.
Physiological Changes #
• Pruritus
• Increases in vascular permeability
• Vasodilation, leading to hypotension, and tachycardia
• Respiratory smooth muscle contraction
• Stimulation of the autonomic nervous system
• Mucus secretion
• Enhanced gut motility
• Platelet aggregation
• Recruitment of inflammatory cells
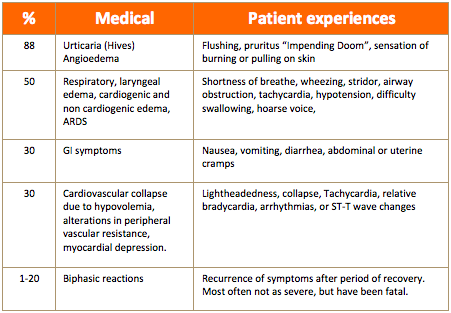
Signs & Symptoms #
- Urticaria (hives) & pruritus
- Angioedema
- Extreme anxiety -> “Impending Doom”
- Pulmonary edema -> bronchospasm, dyspnea, stridor, chest pain
- Hypotension
- Tachycardia -> bradycardia
- Cyanosis
- Cardiovascular collapse
- Nausea, vomiting & diarrhea
- Loss of consciousness
Hives

Laryngeal Edema
Bronchospasm
Diagnosis #
- Acute onset within minutes to a few hours after exposure to an agent known to provoke Anaphylaxis
- Obtain history
- Exclude other conditions
- Labs & Diagnostics
• Can obtain serum for histamine & tryptase
• 24 hr urine for N-methyl histamine
• Skin testing = with allergy specialist and delayed for at least 4 weeks post event.
Treatment #
Must be immediate!
• Call for HELP
• Remove antigen
• ABCs
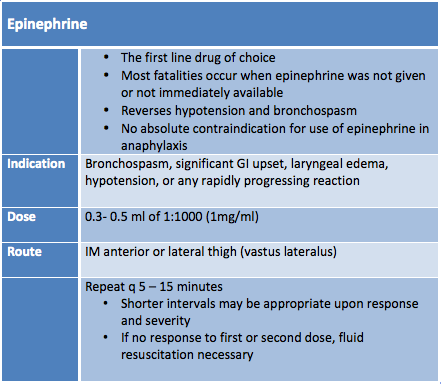
• Epinephrine
ABCs
• Airway & Breathing
• Oxygen
• Prepare for possible intubation -> perform immediately if stridor or respiratory arrest
• Emergent cricothyroidotomy may be required
• Do NOT put a pillow behind their head
• It may obstruct their airway
• Circulation
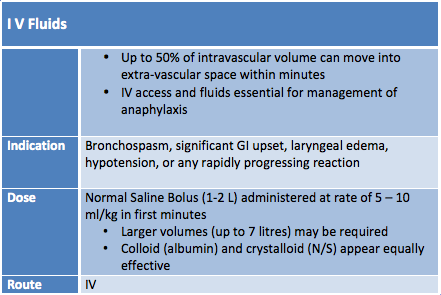
• IV access -> 2 large bore IVs, Normal Saline rapid infusion
Position
• Recumbent with limbs elevated if tolerated
• Most with extreme bronchospasm prefer upright.
Monitor Cardio/pulmonary status
• Frequent vital signs, pulse oximetry
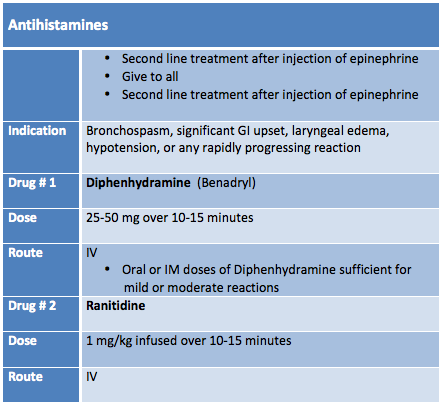
Drugs #
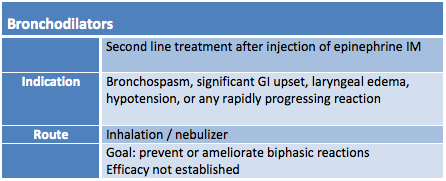
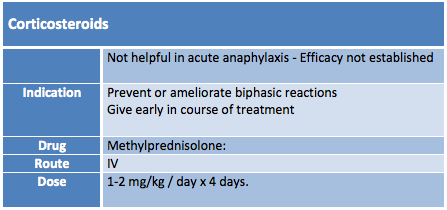
• Epinephrine, IV fluids, antihistamines, bronchodilators, corticosteroids
Prevention #
• Avoidance
• Immunotherapy for hymenoptera allergy
• Pre-medication with antihistamines and corticosteroids before future radiographic contrast media administration
• Antibiotic desensitization
• Epipen = single dose syringe – inject immediately
• Medic Alert Bracelet
Summary #
• Be familiar with pharmacokinetics
• Ask about allergies at booking and prior to administration
of any medication
• Document allergy reactions or sensitivities
• Recognize and manage correctly
• Document