Description #
This unit will describe the correct administration, scoring and interpretation of the LEFS for TJA patients.
Learning Objectives #
By the end of this unit, the learner will be able to perform the following tasks for TJA patients:
– Administer the LEFS
– Score the LEFS
– Interpret LEFS
What is this test? #
What is the LEFS? #
The Lower Extremity Functional Scale (LEFS) is a valid, reliable, and responsive measure for assessing TJA patients and falls within the WHO’s ICF domains of Activity and Participation (Figure 1). The LEFS assesses the patient’s current ability (i.e. what they are able to do today) to perform everyday tasks, specifically activities at home, work, and school, as well as during recreation, and sport. While it is a comprehensive 20 item test, it can be completed and scored in relatively little time (~ 5 minutes).

Figure 1. The International Classification of Functioning, Disability and Health (ICF) Conceptual Model. Taken from Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. Figure 2-1.
When do I use it? #
When do I use the LEFS? #
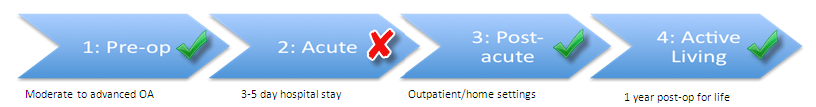
The Lower Extremity Functional Scale (LEFS) can be used in a number of phases along the TJA Continuum of Care. Specifically, as seen in Figure 2, the LEFS is recommended for use in the Pre-Operative, Post-Acute, and Active Living phases of the TJA continuum. Health professionals can therefore use this outcome measure to monitor change in the patient’s status as he or she moves through these phases of the care (*note that it is not recommended in the Acute phase).
Figure 2. The phases along the TJA Continuum of Care for which the LEFS is recommended.
Equipment needed? #
What equipment is used to complete the LEFS? #
To complete the LEFS, the patient will require two pieces of equipment:
- Paper copy of the LEFS
- A pen
A paper version of the LEFS that you can download and print, can be found at the link below.
Please bookmark this link on your web browser so you can access the LEFS when you need it.
How do I do it? #
How do I administer the LEFS? #
Since this is a patient reported outcome measure there is very little that you need to do. Just ensure that the patient has access to the LEFS and have them follow the instructions at the top of the page. When they are finished it will then need to be scored.
- Do you want all the module information on a single piece of paper? If so, click this link → LEFS One Pager
How do I score it? #
How do I score the LEFS? #
Scoring the Lower Extremity Functional Scale (LEFS) is easy to do:
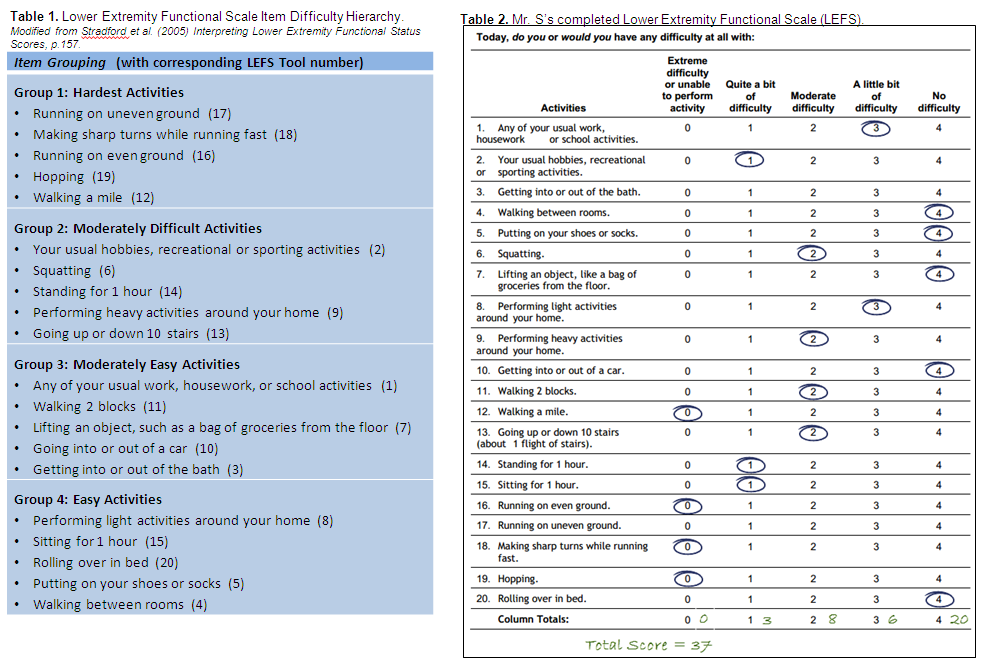
- All items are scored on a 5 point Likert Scale (0-4)
- The columns on the scale are summed to get a total score, with the maximum score being 80.
Data Tips! #
What do I do when items are left blank or when multiple values are circled? #
In some instances, your patient may have left items blank on the Lower Extremity Functional Scale (LEFS). Not to worry! Here are some guidelines from Stratford et al. (2005) for addressing missing values.
- A minimum of 16 items must be answered to use the LEFS
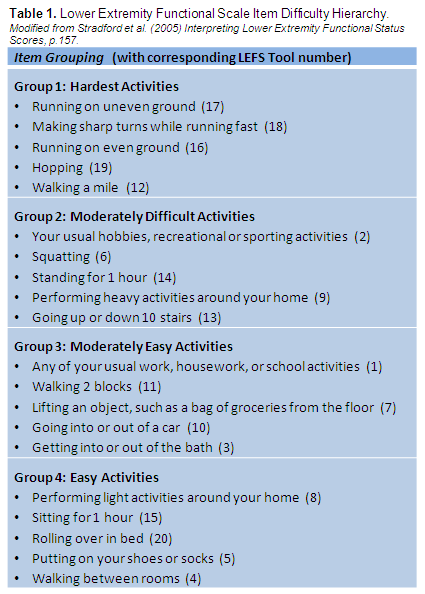
- No more than two missing items can come from any one group reported in Table 1.
- To impute an item score, average the items values provided by the patient for the two closest items identified in the item hierarchy in Table 1.
- If the most difficult item response (running on uneven ground) is missing, assign the score of the closest answered item.
- If the easiest item response (walking between rooms) is missing, assign the score for the closest answered item.
There may also be some instances of a patient circling multiple numbers for a single item. Not to worry! Here are some suggestions that you can use to determine a value for those items.
- You can take the LEFS back to the client and encourage them to select just one value.
- Take an average of the two circled items to get a single value.
- Flip a coin as it is an unbiased method of assigning value.
Example #
Mr. S recently had a left THR and is currently being treated by you in outpatient rehabilitation. You have decided to use the Lower Extremity Functional Scale (LEFS) as your patient reported outcome measure (PROM). When Mr. S hands the LEFS form back, you notice that he left the some items blank. Use the information in Data Tips! as well as Table 1 and Table 2 below to assist you in answering the following questions.
1. Can you use Mr. S’s LEFS even though he has not completed some items?
2. How would you assign a value for the missing items?
– The answers to the above questions can be found below the tables.
Answers #
1. Can you use Mr. S’s LEFS even though he has not completed two items?
- Yes. So long as a minimum of 16 items are answered, then the LEFS can be used.
2. How would you assign a value for the missing items?
- To assign a value to the missing item “running on uneven ground”, assign the score of the closest answered item from Table 1. In this case, we see that “making sharp turns while running fast” is the closest answered question in Table 1. Therefore, we assign a value of 0 to the item “running on uneven ground”.
- To assign a value to the missing item “getting in or out of the bath”, average the item values provided by the patient for the two closest items identified in the item hierarchy in Table 1. In this case, you would average the responses for “getting in or out of a car” and “performing light activities around the home” which have the respective scores of 4 and 3. Therefore, the assigned item value for “getting in or out of the bath” would be 3.5.
What does it mean? #
How do I interpret the LEFS? #
It is simple to interpret the Lower Extremity Functional Scale (LEFS) – the higher the score, the better the patient’s function. For example, a score of 0 indicates extreme disability while a score of 80 indicates no disability. Furthermore, did you know that TRUE CHANGE can be indicated by a increase of 9 points or more? It’s true! It has been established that the:
MDC is 9 points in patients with THA and TKA1
- What does this mean for my patient? It means that in patients with THA and TKA, the change in score between test occasions must be greater than 9 points in order to reflect a true change and not just measurement error.
MCID is 9 points in patients with THA and TKA1
- What does this mean for my patient? It means that in patients with THA and TKA, the change in score between test occasions must be greater than or equal to 9 points in order to indicate that a clinically meaningful change has occurred.
Examples #
Mr. S recently had a right THA and returned home from hospital. Mr S. was referred to community PT and on initial assessment, his LEFS score was 8/80. After 4 weeks of treatment, the PT reassessed Mr. S and his LEFS score improved to 21/80. Knowing the following information:
Please determine if:
- True change has occurred
- Clinically meaningful change occurred.
Has true change occurred? #
To determine if true change has occurred, you must determine if the change between test occasions is greater than the MDC of 9 points.
1. Calculate the change in score between test occasions
2. Compare the MDC to the change in score between test occasions
13 > 9
Yes, the change in score is between test occasions is greater than 9 points and therefore true change occurred rather than a measurement error.
Has clinically meaningful change occurred? #
To determine if clinically meaningful change occurred, you must determine if the change between test occasions is greater than the MCID of 9 points.
1. Calculate the change in score between test occasions
2. Compare the MCID to the change in score between test occasions
13 > 9
Yes, the change in score between test occasions is greater than 9 and therefore clinically meaningful change has occurred.
References #
- Binkley JA, Stratford PW et al. The Lower Extremity Functional Scale (LEFS): Scale Development, Measurement Properties, and Clinical Application. Phys Ther. 1999;79:371-83.
- Finch E, Brooks D et al. Physical Rehabilitation Outcome Measures: A Guide to Enhanced Clinical Decision Making (2nd Edition) Canadian Physiotherapy Association, Toronto ON, 2002.
- Stratford PW, Binkley JM, et al. Validation of the LEFS on patients with total joint arthroplasty. Physiother Can 2000;52:97-105
- WHO International Classification of Functioning, Disability, and Health – http://www.who.int/classifications/icf/icf_more/en/
- Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. F.A. Davis Company: Philadelphia.
- Stratford PW, Hart DL, et al. Interpreting Lower Extremity Functional Status Scores. Physiother Can 2005; 57(2): 154-162
- Paul Stradford, e-mail message to author, February 4, 2015.
