Description #
This unit will describe the correct administration, scoring and interpretation of the 30 sec-CST performed for TJA patients.
Learning Objectives #
By the end of this unit, the learner will be able to perform the following tasks for TJA patients:
– Administer the 30 sec-CST
– Score the 30 sec-CST
– Interpret the 30 sec-CST
#
What is the 30 sec-CST? #
The 30 sec-CST is a valid1, reliable2,3, and responsive2,4 measure for THA and TKA patients that measures functional lower limb strength and dynamic balance through repeated sit-to-stand activity2,5. In addition, the 30 sec-CST falls within the WHO’s ICF domains of Body Function/Structure and Activity and can be completed relatively quickly requiring approximately 2 minutes to administer and score8.
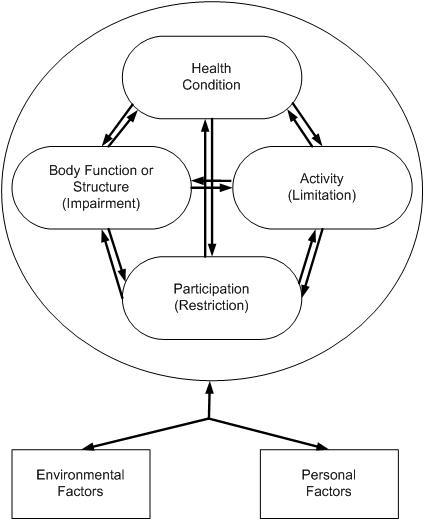
Figure 1. The International Classification of Functioning, Disability and Health (ICF) Conceptual Model. Taken from Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. Figure 2-19.
When do I use the 30 sec-CST? #
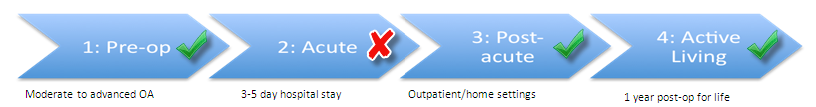
The 30 sec-CST can be used in a number of phases along the TJA Continuum of Care. Specifically, as seen in Figure 2, the 30 sec-CST is recommended for use in the Pre-Operative, Post-Acute, and Active Living phases of the TJA continuum. Health professionals can therefore use this outcome measure to monitor change in the patient’s status as he or she moves through these phases of the care (*note that it is not recommended in the Acute phase).
Figure 2. The phases along the TJA Continuum of Care for which the 30 sec-CST is recommended.
What equipment is used to perform the 30 sec-CST? #
To perform the 30 sec-CST with a patient, the following pieces of equipment are required2,5,6:
- Straight back chair with a 43-46 cm seat height and no arm rests. Place the chair backed against the wall to prevent slipping.
- Stopwatch or a timer.
REMEMBER!
- Whenever possible, the same chair should be used for re-testing.
How do I administer the 30 sec-CST? #
To learn how to administer the 30 sec-CST, please review the instructional video below.
How do I score the 30 sec-CST? #
Scoring the 30 sec-CST is simple to do:
- Record the total number of stands (up and down equals one stand) completed in 30 seconds.
If the patient is unable to stand from sitting, then the score for the test is zero2.
REMEMBER!
- Only include in the stands in which the patient starts in a seated position, stands fully erect, and returns fully to the seated position. If at the 30 second mark the patient has completed a full stand (i.e. standing fully erect or is on the way down to the sitting position), then this final stand is counted in the total5.
- If the patient uses their arms to push off or they do not stand in the fully erected position, then these incomplete efforts should not be included in the total number counted6.
How do I interpret the 30 sec-CST? #
To interpret the 30 sec-CST is simple: the more repetitions that the patient can complete in 30 seconds the better. Furthermore, did you know that TRUE CHANGE is indicated by an improvement of only 1.6 repetitions? It’s true! It has been established that the:
MDC 90 is 1.6 repetitions in patients with hip OA4 and those awaiting TJA of the hip and knee6.
- What does this mean for my patient? It means that in patients with hip OA and those awaiting TJA of the hip and knee, the change in score between test occasions must be greater than 1.6 (mean value for a group of patients) or 2 (for an individual patient) in order to reflect a true change and not just measurement error.
MCII ranged from 2.0-2.6 stands in 30 seconds in patients with hip OA4.
- What does this mean for my patient? It means that in patients with hip OA, that the change in score between test occasions must be greater than 2.6 (mean value for a group of patients) or 3 (for an individual patient) in order to indicate that a clinically meaningful change has occurred.
PASS cut off point with hip OA after 9 weeks of physiotherapy is ≥ 11 stands7.
- What does this mean for my patient? It means that in patients with advanced hip OA, the number of chair stands must be greater than or equal to 11 after a course of physiotherapy treatment in order for patients to likely be satisfied with their functional status.
ADDITIONAL RESOURCES
- The 30- sec Chair Stand Test can most reliably be compared to normative values if the seat height of the chair used measures 43 cms. If you would like more information regarding normative values for different patient subgroups as well as criterion-referenced fitness standards to maintain physical independence in moderately active older adults, then click on this link to Rehab Measures.
Examples #
Mr. S has hip OA and is awaiting THA surgery. He has come to your clinic to improve his strength and balance prior to his surgery. On initial assessment, you have Mr. S perform the 30 second Chair Stand Test (30 sec-CST) in which he scores 9 reps. After 9 weeks of treatment, you reassess Mr. S’s 30 sec-CST and he scores 17 reps. Please determine if:
- True change has occurred
- Clinically meaningful improvement has occurred
- Mr. S is likely satisfied with his functional status
Has true change occurred? #
1. Calculate the change in score between test occasions
17 reps – 9 reps = 8 reps
2. To determine if true change has occurred, compare the MDC to the change in score between test occasions. *MDC = 1.6 reps (or 2 reps for individual patients)
8 reps > 2 reps
Yes, true change has occurred as the change in score between test occasions is greater than the MDC of 2 reps.
Has clinically meaningful change occurred? #
1. Calculate the change in score between test occasions
17 reps – 9 reps = 8 reps
2. To determine if clinically meaningful improvement has occurred, compare the MCII to the change in score between test occasions. *MCII = 2.0-2.6 (or 3 for individual patients)
8 reps > 2 reps
Yes, clinically meaningful improvement has occurred as the change in score between test occasions is greater than the MCII of 3 reps.
Will Mr. S be satisfied with his functional status? #
1. To determine if Mr S would be satisfied with his functional status, compare the PASS score to the Mr S’s post treatment score. *PASS = ≥ 11 reps
17 reps > 11 reps
Yes, Mr S. likely satisfied with his functional status as his post treatment score is greater than the PASS of 11.
References #
- Gill SD, de Morton NA, Mc Burney H. An investigation of the validity of six measures of physical function in people awaiting joint replacement surgery of the hip or knee. Clin Rehabil. 2012;26(10):945-51.
- Dobson F, Bennell KL, et al. Recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthritis Cartilage 2012; 21(8):1042-52. Available from: www.oarsi.org/sites/default/files/docs/2013/manual.pdf
- Gill S, McBurney H. Reliability of performance-based measures in people awaiting joint replacement surgery of the hip or knee. Physiother Res Int. 2008;13(3):141-52.
- Wright AA, Cook CE, et al. A comparison of 3 methodological approaches to defining major clinically important improvement of 4 performance measures in patients with hip osteoarthritis. J Orthop Sports Phys Ther. 2011;41(5):319-27.
- Bennell K, Dobson F, Hinman R. Measures of physical performance assessments. Arthritis Care Res 2011;63(Suppl 11):S350-70.
- www.rehabmeasures.org/Lists/RehabMeasures/PrintView.aspx?ID=1122
- Emerson Kavchak AJ, Cook C et al. Identification of cut-points in commonly used hip osteoarthritis-related outcome measures that define the patient acceptable symptom state (PASS). Rheumatol Int 2013;33:2773-82.
- WHO International Classification of Functioning, Disability, and Health – http://www.who.int/classifications/icf/icf_more/en/
- Riddle, D. & Stradford, P. (2013). Is this Change Real? Interpreting Patient Outcomes in Physical Therapy. F.A. Davis Company: Philadelphia.
