Description #
This unit is designed to help the students and clinically registered nurses develop a better understanding of the skills involved in tracheostomy care.
Learning Objectives #
Upon completion of this module you will be able to:
- Describe the indications for a tracheostomy tube
- List complications seen with tracheostomy tubes
- Identify common features of a tracheostomy tube
- Follow the standards of care for a tracheostomy patient
- Demonstrate the steps required for weaning from a tracheostomy tube
- Explain the emergency procedures to follow for a tracheostomy patient
Introduction #
TRACHEOSTOMY CARE
This unit is designed to help you understand the principles and skills involved in tracheostomy care.
A tracheostomy (also known as a tracheotomy) is a surgical procedure performed on the neck to open a direct airway through an incision in the trachea. Tracheostomy can also refer to the result of the procedure, i.e. the opening itself). Tracheostomy is a commonplace surgical procedure for maintaining an airway in cases of obstruction. Clients with tracheostomies may may be found in both acute hospital and community settings, and tracheostomies may be permanent or temporary in their nature.
Technically, the term “tracheotomy” from the Greek root tom- meaning “to cut,” refers to the procedure of cutting into the trachea, whereas the term “tracheostomy”, with the root stom- meaning “mouth,” refers to the procedure of making a semipermanent or permanent opening.
The Indications for a Tracheostomy #
A tracheostomy is a surgically created opening through the front of the neck and into the trachea below the level of the larynx. The opening is usually made between the 2nd and 3rd tracheal rings.
Tracheostomies are best performed as an elective procedure when the airway has already been stabilized via an endotracheal tube. The procedure is generally performed in the operating room under a general anesthetic, although it is occasionally done as an emergency procedure to establish an open airway. It may also be done percutaneously at the bedside.
Specific indications for tracheostomies are:
1. To alleviate upper airway obstruction
Obstruction of the upper airway that is not easily removed will be alleviated by making a surgical airway below the level of the obstruction. Examples include foreign bodies lodged in the trachea, a tumor obstructing ventilation, and vocal cord paralysis.
2. To provide long term ventilation
Patients who are intubated for longer than 2 weeks with spinal cord injury or progressive neuromuscular weakness often require tracheostomy tubes to facilitate long-term ventilation. Endotracheal tubes are not considered long-term or permanent airways as they are not well tolerated by the awake patient and can cause pressure sores or mucosal damage to the lips and surrounding tissues. They are also difficult to keep well secured and impede oral hygiene.
3. To facilitate the removal of secretions
Patients who are unable clear pulmonary secretions can require a tracheostomy to facilitate tracheal suctioning. This is often the case with patients who are unable to cough effectively due to muscle weakness or diaphragm paralysis, patients who will not cough due to a decreased level of consciousness, or patients with excessive secretions such as severe bronchiectasis, cystic fibrosis, or pneumonia.
4. To protect the airway
Patients with a decreased level of consciousness are not able to protect their airway with a gag reflex or position themselves to keep their soft tissues or tongue from blocking their respiration. These patients are often intubated, but if the decreased level of consciousness is due to a more permanent condition such as a head injury or stroke, they sometimes require a tracheostomy. Tracheostomies are sometimes necessary for airway protection with people who have had severe facial trauma.
The Complications Seen With Tracheostomy #
Tracheotomy is a well tolerated surgical procedure with a mortality rate reported anywhere from 0.9% to 5.1%. There are 2 categories of complications that are seen with tracheostomy procedures or tracheostomy tubes:
1. Immediate complications
- Hemorrhage
- Pneumothorax: most often occurs in children and COPD, from lacerating the apex of the lung during surgery
- Subcutaneous and mediastinal emphysema: resulting from air tracking through tissues from open trachea
- Respiratory and cardiovascular arrest: could result from asphyxia during the surgical procedure or cardiac arrythmias
2. Late complications
- Airway obstruction:resulting from a tube migrated out of position or from thick dried secretions
- Infection: ineffective clearance of secretions. Patient may be immunocompromised or may have nosocomial pneumonia, signs include redness, discharge, crusting at the stoma, increased secretions or thicker than usual mucus
- Aspiration: caused by impaired cough and gag reflex or an inadequate seal between the cuff and the trachea
- Tracheal erosion
- Tracheoesophageal fistula: caused by having a hyperinflated cuff impinging on a nasogastric tube or oral feeding with an inflated cuff.
- Tracheo-innominate fistula: erosion through the anterior tracheal wall into the innominate artery (the innominate artery crosses the surface of the trachea at the level of the upper sternum). Life threatening and immediate surgery is required. The tracheostomy tube is replaced with an endotracheal tube and finger pressure held against the fistula.
- Tracheal Lesions
- Tracheal granulomas: form in the trachea in proximity to the tip of the tube and are likely related to the movement of the tube
- Tracheomalacia: the softening of the cartilagenous rings resulting in the collapse of the trachea during inspiration
- Tracheal stenosis: a narrowing of the lumen of the trachea, which can occur as the tracheal rings start to heal. Fibrous scarring causes the airway to narrow. Stenosis may occur at the cuff site or the tip of the tube, but most often occurs at the stoma site. The stenosis at the stoma site may be caused by stomas that are cut too large, infection of the stoma, movement to the tube, or frequent tube changes.
Common Features of the Tracheostomy Tube #
Standards of Care for a Tracheostomy Patient* #
Patients with tracheostomy tubes should receive thorough patient assessments. Particular attention should be paid to the respiratory assessment with an assessment of breath sounds, pulse oximetry, respiratory distress, and suctioning as needed.
Cuff Pressures:
Tracheostomy cuff pressures should be checked each shift. This may be done by a Respiratory Therapist at your site. The pressure inside a tracheal cuff should be kept below 30 cmH20 to avoid damage to the tracheal mucosa. If a tracheostomy cuff must be inflated with air and a cuff pressure measurement device is not available, attach a syringe and inflate the pilot balloon with the smallest volume of air required to stop the air leak (<5 cc).
Tracheostomy Dressing Changes:
Tracheostomy dressings should ideally be changed Q8 hours and PRN. Check your policies for guidelines.
Inner Cannula Cleaning and Changes:
All inner cannulas should ideally be changed Q24 hours and PRN. Check your policies for guidelines. Inner cannulas may be disposable or non-disposable. The inner lumen of these cannulas can be removed and soaked or cleaned with normal saline and sterile q-tips. Use half strength hydrogen peroxide diluted with normal saline only when dried mucous/encrustations cannot be removed from the plastic surfaces with saline alone. If hydrogen peroxide is used for cleaning, ensure the inner cannula is thoroughly rinsed in saline before reinsertion.
Tracheostomy Tie Changes:
Tracheostomy tube ties should be changed PRN when visibly soiled. Tubes are usually secured with soft foam hook and loop fasteners. When changing ties, it is safest to attach new ties before removing the old ones to avoid accidental decannulation. If the ties must be removed before attaching the new ones, a second person must be available to hold the tube securely throughout the procedure.
Tracheostomy Tube Changes:
The first tracheostomy tube change following surgery is usually done by a physician or Respiratory Therapist to ensure the stoma is in satisfactory condition and to remove any stitches. Tubes are changed regularly every 2 weeks to 4 weeks depending on specific hospital guidelines. Tubes can also be changed PRN for:
- changing the type of tube (e.g. cuffed to cuffless)
- replacement of ineffective or malfunctioning tubes
- downsizing of tube for weaning purposes
Weaning From the Tracheostomy #
Weaning from a tracheostomy tube is a multi-step procedure, with the ultimate goal being decannulation. It requires careful attention and coordination of the health care team, and is very patient specific. Weaning from a tracheostomy tube can take anywhere from several days to several months to decannulation. RN’s should be familiar with the tracheostomy weaning process at their site (see sample flowchart) and may be required to assist with plugging trials or cuff deflation trials.
Emergency Procedures to Follow for the Tracheostomy Patient #
All patients with a tracheostomy tube or open stoma usually require the following emergency equipment at their bedside. Check your hospital policies for site-specific guidelines:
a. suction equipment
b. oxygen equipment (including a humidification device)
c. emergency tracheostomy equipment bag containing:
- replacement cuffed tracheostomy tubes (one of the same size, and one a size smaller
- obturator and spare inner cannula for tube insitu
- 10 ml syringe
- tracheal tube exchanger
- tracheal dilator set
- package of water soluble lubricant
Complications involving a patient’s airway can quickly become life-threatening. All staff working with tracheostomy patients should be trained to respond immediately to these emergencies and deal with them appropriately.
Hemorrhage:
Hemorrhage from a tracheostomy incision is generally only a complication that occurs within the first 24-48 hours post surgery. Steps taken to assess and treat hemorrhage include:
- assess stoma for bleeding (a small amount of blood in the first 24 hours is normal)
- report any swelling in the surrounding tissues of the neck
- report vigorous pulsation around the trachea (may indicate impending innominate artery rupture)
If hemorrhage occurs:
- inflate cuff immediately (if present) to 25 cmH20
- suction through tracheostomy tube and mouth if necessary
- notify physician
- monitor vital signs
- apply pressure if possible
Tube Occlusion:
Tracheostomy tubes rarely occlude completely if care and maintenance policies are followed. Patients should be kept well hydrated to minimize thick secretions, inspired gases should always be humidified, and suctioning should occur regularly and as needed. Instillation with sterile saline during suction procedures should be done to thin secretions if necessary. Stoma sites should be kept clean and inner cannulas removed, cleaned and replaced as per guidelines. If the tube occludes:
- remove inner cannula
- encourage patient to cough
- if unsuccessful, instill sterile saline and attempt to pass a suction catheter through blocked tube
- if unsuccessful, cut tie tapes, remove entire tracheostomy tube, insert tracheal dilators and hold stoma open
- call a code blue and prepare for a tube change
- insert new cuffed tracheostomy tube, inflate cuff and attempt to ventilate if patient is not breathing
Accidental Decannulation:
Tracheostomy tubes rarely fall out on their own if proper care is taken to keep them well secured. Tubes can be tied with twill tapes around the neck, but soft Velcro ties are more comfortable and more commonly used for long-term tracheostomies. Ties can be loosened to clean underneath but should not be removed unless the tracheostomy tube is held in place at all times manually. For procedures in which the ties must be removed (i.e. tube change) there should always be two people present so that the tube can be held in place for the duration of the procedure. Patients who are considered at risk to pull their tracheostomy tubes out may need to be physically restrained to prevent loss of airway.
The following steps describe the procedure to follow for an accidental decannulation:
- If patient is not breathing, cover stoma and ventilate with mask and bag connected to oxygen
- Call a Code Blue
- Prepare emergency airway equipment for re-insertion
- Prepare client for re-insertion by laying patient flat and hyperextending neck to open stoma
- Prepare tracheostomy tube for insertion (lubricate and insert obturator)
- Use tracheal dilators to open stoma if needed
- Insert trach tube from side of stoma while rotating toward midline
- Remove obturator and replace with inner cannula
- Reconnect to ventilator or bagger if required
- Auscultate to check for correct placement
Aspiration #
It is possible for tracheotomy patients to eat and drink fluids, but normally they will first be changed to a cuffless tracheostomy tube or have their cuff deflated before attempting swallowing. An inflated cuff can interfere with the normal swallowing mechanism. Patients should be assessed by a Speech-Language Pathologist or Occupational Therapist for swallowing ability before having food or beverages to prevent aspiration. Tracheostomy patients having oral fluids should be alert, with a good swallow and gag reflex.
Prior to food or beverages, the tracheostomy patient should be maintained in a high Fowler’s position. If the patient is at risk for aspiration, inflate cuff for a period of time after meals, or as ordered.
Watch for the following signs and symptoms of aspiration:
- excessive coughing
- gagging
- increased secretions
- presence of ingested food in tracheal aspirate
- decreased oxygen saturation
- if you suspect a patient has aspirated, inflate the cuff immediately, ventilate if necessary, and suction through the tracheostomy tube as well as orally. Leave cuff inflated and call physician, and/or inform the Respiratory Therapist.
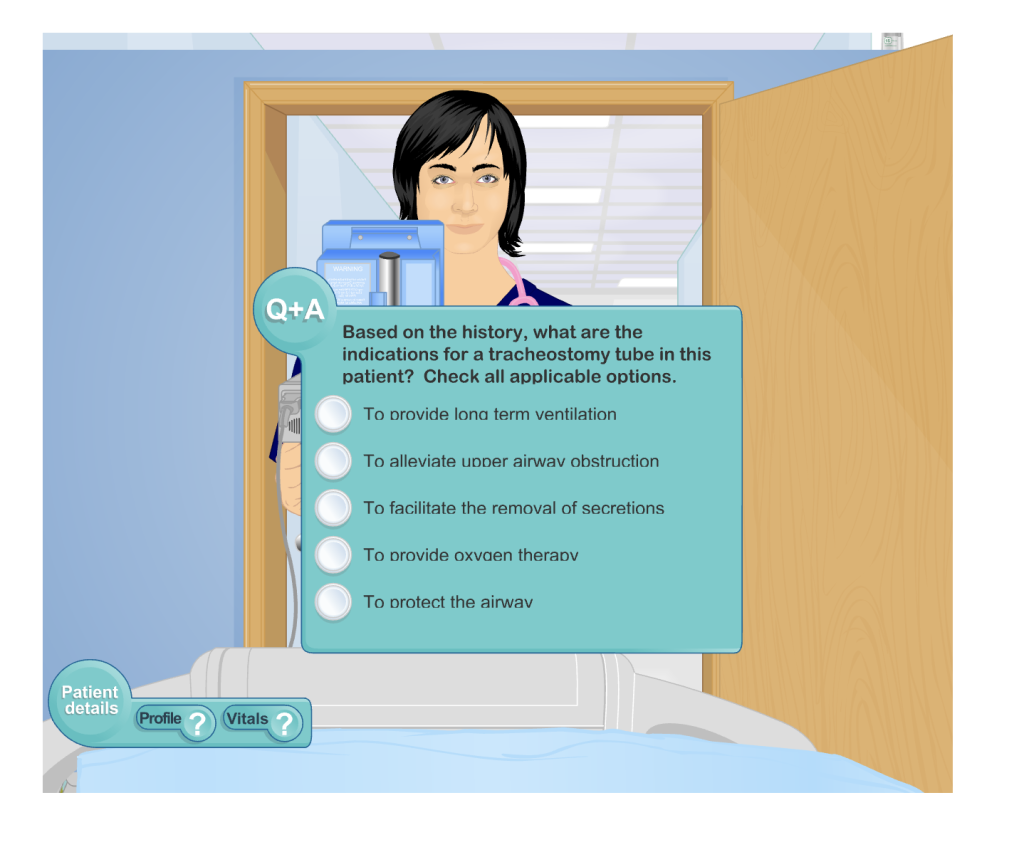
Tracheostomy Simulation #
The screen below is an interactive simulation that explores the management of tracheostomy in the acute clinical setting.
References #
- Vancouver Acute Patient Care Guidelines T-150 Tracheostomy: Care and Management of a Patient with a Tracheostoma. 2007.
- Vancouver Acute Patient Care Guidelines T-155 Tracheostomy Tube Changes. 2007.
- Vancouver Acute Patient Care Guidelines T-160 Tracheostomy: Changing the Tie Tapes. 2007.
- Vancouver Acute Patient Care Guidelines T-165 Decannulation. 2007.
- Vancouver Acute Patient Care Guidelines T-170 Tracheostomy Tubes – Cuff Deflation. 2007.
- Vancouver Acute Patient Care Guidelines T-180 Tracheostomy: Cuff Pressure, Measurement and Maintenance. 2007.
- Vancouver Acute Patient Care Guidelines T-190 Tracheostomy: Dressing Change and Inner Cannula Cleaning. 2007.
- Vancouver Acute Patient Care Guidelines T-195 Tracheostomy – Suctioning. 2007.
- Vancouver Acute Patient Care Guidelines T-200 Tracheostomy: Plugging. 2007.
- Vancouver Acute Patient Care Guidelines R-265 Cuff Pressure. 2007.
- Vancouver Acute Patient Care Guidelines R-370 Emergency Airway Equipment (includes Laryngectomy and Open Stoma Patients). 2007.
- Vancouver Acute Respiratory Services CBE of Tracheostomy. Sasse B, McKeown, SI.
- Vancouver Acute Tracheostomy Weaning Flowchart.
- Vancouver Acute: Tracheostomy Tube Management – Quick Reference Guide.
- Vancouver Acute: Managing the Adult Tracheostomy Patient. Hohndorf, S.
